
Medical errors are cited among the leading causes of death in the United States, resulting in devastating consequences for patients and their families, besides adding substantial costs to healthcare. Communication within and between teams is cited as a major contributing factor to patient deaths due to preventable medical errors. Although Universities and Academic Health Centers aim to graduate competent healthcare professionals who are effective healthcare team members, the importance and degree of emphasis given to interprofessional education (IPE) across health professions accreditation organizations is variable. To ensure a highly skilled, efficient and confident health professions workforce, an interprofessional, experiential, performance-based model for health professions education is proposed. This transformational model must be relevant for this high-risk, data-driven and increasingly technological medical era. Finally, it must revolve around patient safety and well-being as patients traverse through the levels of the healthcare system and upon the safety and well-being of professionals providing them care.
Recent studies estimate between 210,000 and 400,000 deaths annually are due to preventable medical errors [1]. These include wrong diagnoses, drug dosage miscalculations, hospital-acquired infections, falls, treatment delays and miscommunication among and between healthcare teams [1]. Due to several factors, these numbers could be underestimated. Patient outcomes are not entirely dependent on individual caregivers [1,2]. Faulty methodologies and inconstancy of reporting errors are identified as a legitimate concern [1]. The annual cost of medical errors to the U.S. economy may reach one trillion dollars a year [2]. Even if they do not result in the actual loss of lives, hospital-related errors can have inestimable, long-lasting and costly effects on individuals, families and society [1]. When it comes to the personal level, one death or permanent injury of a family member is too high a price to pay.
Deaths and injuries due to medical errors are not solely a problem in the United States. According to the World Health Organization (WHO), up to 10% of hospital patients in developed countries may be harmed while receiving care [3]. A study from the United Kingdom reports that 3.6% of hospital deaths were due to preventable medical errors. A study from Norway reported this rate to be 4.2% [4,5]. A meta-analysis published in the British Medical Journal concluded at least 1 in 20 patients is affected by preventable patient harm, with 12% of this group suffering from permanent disability or death [6]. Similar statistics and challenges have been reported in Japan, New Zealand and Australia [7].
In the 21st century, healthcare institutions, accrediting bodies and hospitals have been making significant efforts to improve safety and quality outcomes as avoidable deaths due to medical error have been reported as a national concern, receiving focused attention since the landmark publication by the Institution of Medicine, ‘To Err is Human’ [8]. Hospitals in the United States and around the globe have been implementing various system-based measures, ranging from instituting bar codes for medication dispensing, fall protocols, checklists, chart reviews and ‘no-blame’ reporting mechanisms. Even these efforts are susceptible to breakdowns in systems and processes. Notwithstanding best efforts on the part of healthcare institutions and accrediting bodies, preventable deaths and injuries due to avoidable errors remain highly problematic. Lessons from high-reliability organizations reveal that human factors, such as fatigue and cavalier attitudes, play an important causal role in poor outcomes [9–12]. Healthcare delivery and patient outcomes are not entirely dependent on individual caregivers. Excellent medical outcomes are linked to receiving care from highly functional, interprofessional teams with mature safety and quality systems in which to practice [9,13,14]. Still, the importance and degree of emphasis on interprofessional team functioning remain variable in health professions accreditation requirements and teaching institutions across the different health professions. Paige et al. identified key challenges or barriers to implementing interprofessional education (IPE). These included lack of leadership or champions, faculty who develop appropriate content, addressing the training needs of the learners, logistical issues, including sufficient space, and beliefs and attitudes towards other healthcare professions. Disagreement can also occur between educators representing different specialties, even within the same profession, regarding developing content that can be used universally, as well as a lack of regional and/or national accreditation bodies for IPE courses that can grant continuing education credits [15]. Hence, as educators interested in advancing IPE, we must collaborate to overcome these challenges in order to ensure health professions graduates enter the workforce sufficiently skilled to function effectively as healthcare team members.
Undergraduate and graduate health professions education curricula in many countries face challenges related to the way healthcare professionals have been trained during the latter years of the 20th century [16]. Traditionally, health professions education has relied upon learning by attending lectures, reading and assessing knowledge acquisition by grading patient care skills acquired during clinical rotations experiences. For the most part, the assessment of readiness to progress remains reliant upon either multiple-choice (MCQ) questions, viva (oral boards), and/or written short or long-answer-type questions [17]. Formative evaluation focuses on the learner’s growth and development in the job or field of study, whereas summative evaluation focuses upon a student’s progress in the training program over time. Both formative and summative assessment methods are necessary for health professions educators, credentialing bodies and future employers to determine the competence levels of newly graduated or mid-career healthcare providers [18]. Health professions students are typically very capable of passing summative assessments and year-end qualifying and certifying examinations. However, the current evaluation systems that assess progress throughout clinical training tend towards a subjective approach when assessing procedural skill development and team functioning [19]. Skill acquisition has posed a special challenge for physician training following the reduction in duty hour requirements [20]. While trainees may be more rested and have a better life balance, they are graduating with less exposure to procedures [20,21]. As a result, the current model of training may not predict readiness to safely care for patients [22].
A challenge for health professions educators in the 21st century is how to accomplish a paradigm shift to adopt an interprofessional, experiential performance-based training model. Such a model would carry over a lifetime of practice and prepare for the stresses of the modern healthcare environment. This paradigm shift would improve the outcome of training as well as assure the public that health science colleges and postgraduate/residency training programs are truly producing and credentialing safe healthcare providers.
In an effort to ensure safety and quality in training, credentialing organizations in the United States, as well as other countries, have already embedded changes in accreditation training requirements, including the adoption of competency domains and milestones [23,24]. Nevertheless, obtaining objective measures of each student’s skills remains challenging as they progress through training, including postgraduation and beyond. Clinical competence is ‘a journey of a learner from a novice in the field of his/her scope of practice to achieving expertise in their given field’ [25]. Important competency domains such as professionalism, patient care, clinical knowledge, critical thinking, resource management, system-based practice and communication are already identified and included in most health professions’ accreditation requirements [26]. While the professional competency domains are similar, each healthcare discipline uses different nomenclature. A coordinated, reliable and valid performance-based assessment model, one that allows learners to progress at their own pace while also objectively measuring individual procedural proficiencies, communication and interprofessional team skills, has yet to be fully realized [27,28]. Procedural and interprofessional team skills are rarely assessed in a truly structured and objective manner that assures competence [22,29].
Developing a training model that provides a valid, reliable and objective assessment of performance for health professions has proved challenging [27,28,30]. Among the challenges faced when assessing team performance and competencies, Lingard et al. pointed out that individuals in a team can fail to meet defined competency levels, even though the same interdependent team could collectively perform to meet team competency thresholds. Also, for example, teams may demonstrate competency in one clinical scenario but not necessarily in a different scenario [31].
Health professions accrediting bodies emphasize professional attitudes towards patients and colleagues, including communication and teamwork. For example, ACGME (Accreditation Council for Graduate Medical Education) for physicians, CCNE (Commission on Collegiate Nursing Education) and CAAHPE (Commission on Accreditation for Allied Health Professionals Education) are making significant strides in assessing critical thinking and procedural skills for Board Certification and/or Continuing Education [26,32]. Nevertheless, the predominant model of health professions education still does not routinely assess performance in procedural and interprofessional core competencies nor reliably measure the progress of skills acquisition for individuals or teams. Preparedness for practice is an especially important concept for rural healthcare, where consults with clinical subject matter experts are less readily available. During the early stages of the COVID-19 pandemic, the situation was further compounded, with many clinical training sites becoming inaccessible to students for learning purposes [33,34]. Students and trainees in healthcare education experienced limited clinical exposure, including the cessation of elective surgeries, as well as safety concerns related to exposing trainees to the virus [33,35].
Due to potential delays in diagnosis, skill deficiencies and inefficiencies, the current training model can contribute to avoidable medical errors or be perceived as negligence [36]. Thus, a new graduate from the traditional model of training could potentially enter the healthcare system, offering services that are risky for patients. The intent of this call for the adoption of an interprofessional, experiential, performance-based model for health professions education is to ensure that accredited institutions and programs are graduating students who can demonstrate as well-prepared and ready to function at a high level in the intensity and complexities of modern clinical practice.
To bridge the gap from classroom to clinical experiences, and with the emergence of advanced simulation and visualization technologies, preparatory clinical experiences can be supplemented during training by using methods that fully engage students and practitioners in realistic, experiential (hands-on) learning scenarios. An interprofessional model that embraces simulation-based healthcare education (SBHE) can fulfill many individual and interprofessional team requirements to achieve meeting accreditation competencies for each healthcare discipline [37–39]. Additionally, simulation experiences can offer a wide variety of training, ranging from basic skills, i.e., catheter or tube insertion, to advanced care scenarios, such as managing complex patient emergencies, conducting procedures and rehearsing routine and rare occurrences in authentic, simulated healthcare settings (Figures 1–5) [37–40].

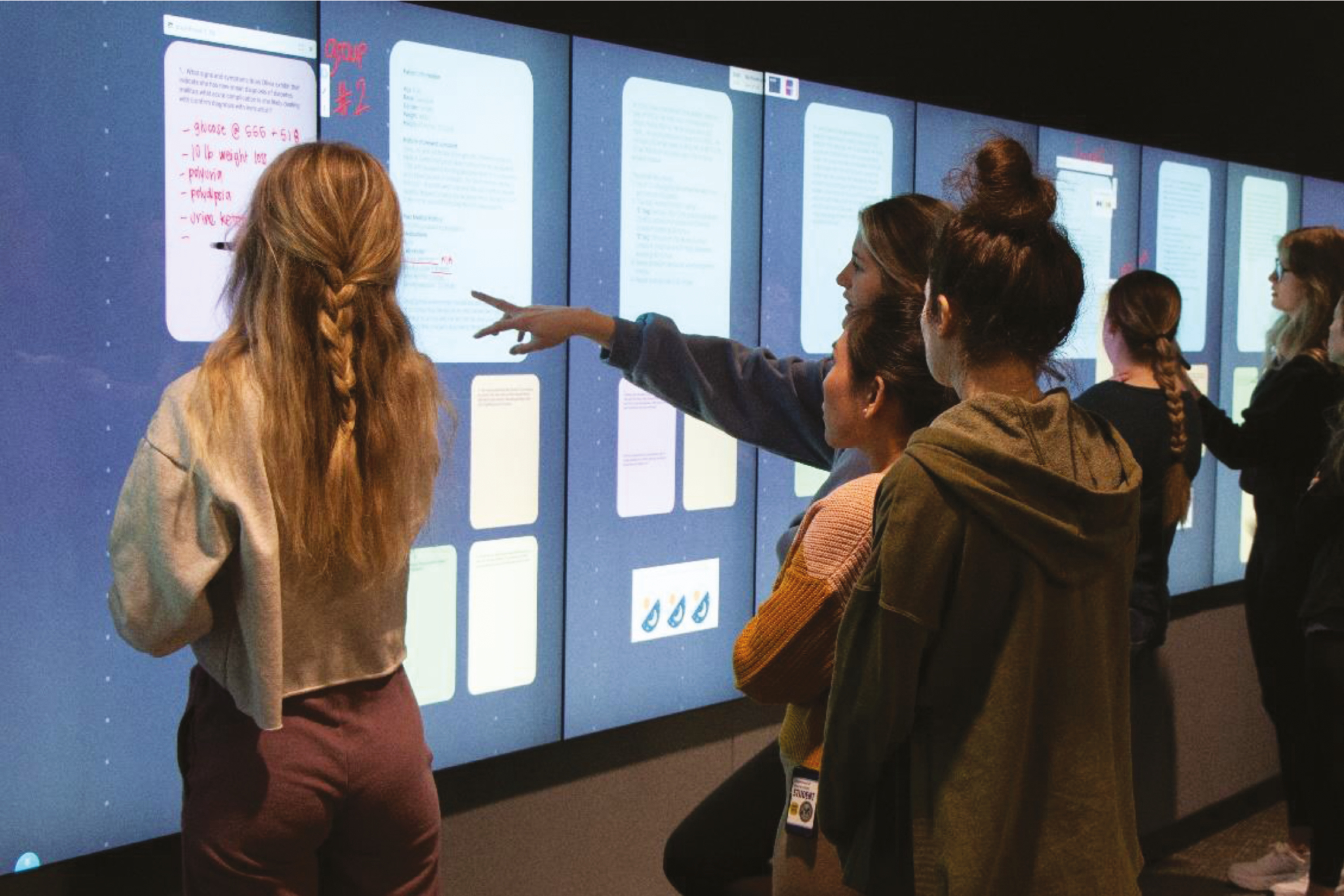
Nursing students collaborate on a case-based exercise using an interactive digital wall


Physician Assistant students managing a patient in a simulated patient scenario


Student practicing phlebotomy skills using a task trainer


Physicians practicing advanced surgical skills in a simulated operating room

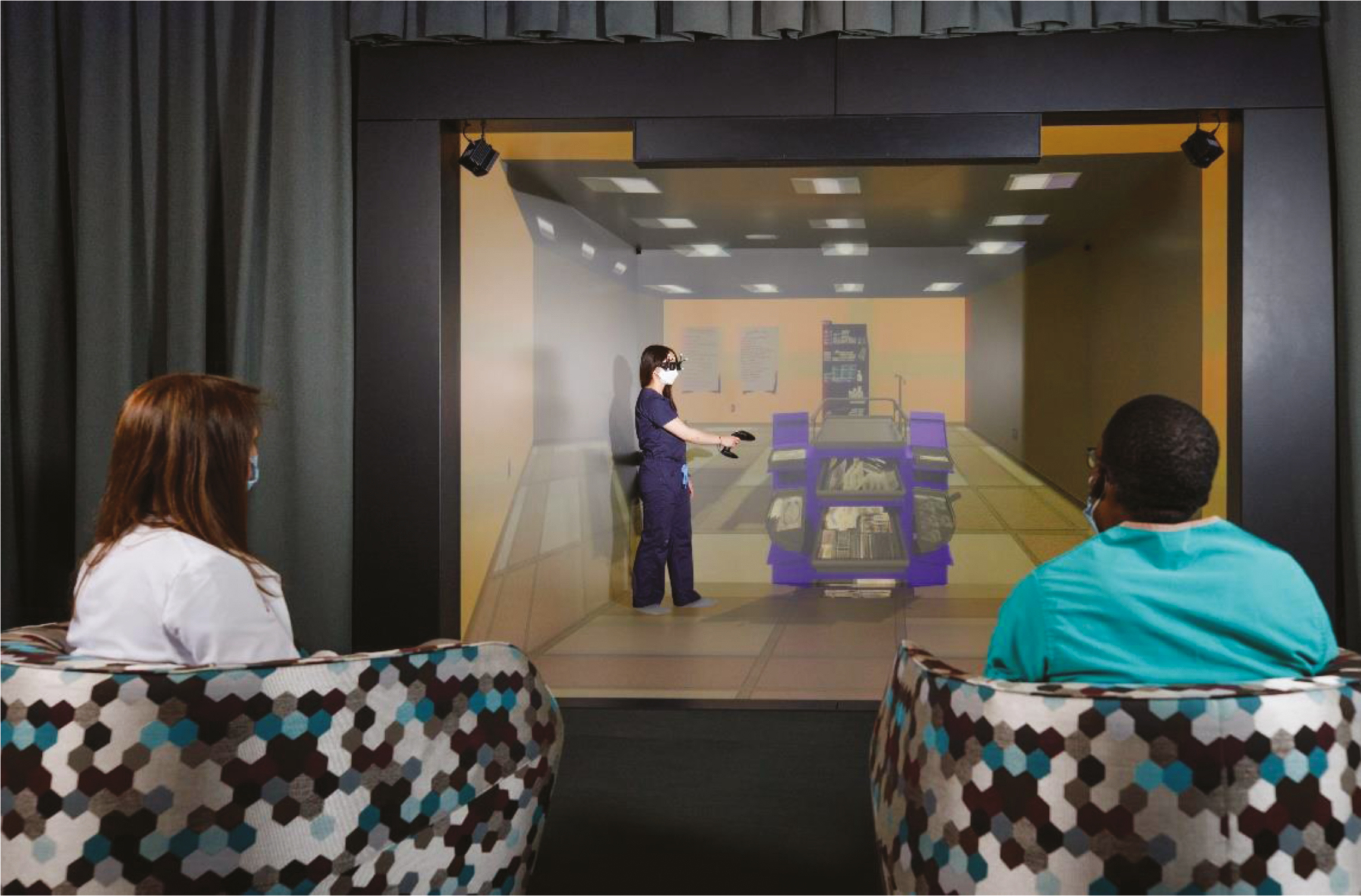
A nursing student exploring a crash cart in a virtual reality immersive 3D CAVE
Many studies support that the incorporation of simulation-based training of intra- and interprofessional healthcare teams results in better clinical care and patient outcomes [41–47]. One recent study, for example, demonstrated a significant reduction in medication errors in intensive care units due to simulation-based IPE [48]. Another study and meta-analysis of randomized controlled trials on interprofessional simulation-based training demonstrated improvement in patient-centric approach to care, collaborative teamwork, communication and professional identity among healthcare students [49,50].
Gaps in the summative and formative evaluation model for graduates can be identified and addressed through the SBME approach [51–53], especially one that emphasizes interprofessional concepts and implements experiential learning. A model that first teaches ‘hands-on’ skills and then offers opportunities to practice until proficiency can be deployed prior to routinely assess and document formative skills development, as well as demonstrate readiness for unsupervised clinical practice (summative). An interprofessional, experiential training approach, which adopts interactive and ‘hands-on’ learning methods using simulation, provides a framework for implementing a shared health professions performance-based training model that still allows for individuality within each discipline. Such an approach assures a focus on IPE and team skills development, confidence building and clinical collaboration. This model will greatly help meet public expectations related to receiving high-quality and safe patient care outcomes.
Health professions educators who supervise trainees in clinical settings will always provide an important safety net for all learners and patients who traverse the healthcare system. However, due to advances in simulation technology, learners can now achieve a defined level of performance without the need to practice on patients. The shift to an interprofessional, experiential, performance-based model is admittedly complex. This approach should use the principles of deliberate practice and mastery learning and include routine assessment of training milestones to ensure readiness for unsupervised medical practice and board certification, hospital privileges or state licensing [54–59].
For successful deployment, this paradigm shift demands purposeful collaboration amongst the healthcare disciplines but also requires the adoption by faculty of different teaching styles and assessment methods. For example, pre-briefing, debriefing and facilitation of simulation activities call for very different teaching skills than delivering knowledge by a lecture with PowerPoint, creating e-learning modules and mentoring learners on rounds [38]. In fact, many lectures can be converted to case-based simulation scenarios during which individual and team competencies can be taught and practiced. Large classes can be divided into small groups for enhanced interactive learning, and clear, measurable objectives can be created to achieve defined educational outcomes. Immersive learning experiences in realistic, replicated healthcare settings can also be successfully used for competency testing and high-stakes examinations, such as licensing examinations for physicians to ensure that they provide competent and safe patient care [9,13,14,18,49].
An interprofessional, experiential, performance-based model for healthcare professionals should be designed to improve objectivity in assessing individual and team performance. This includes starting with the development of an interprofessional and shared team performance domain model that focuses on the ‘hand-off’ from one level of care to the next, where patients are most vulnerable [60,61].
Based upon the concerns identified by Paige et al. [15], and in order to improve patient safety outcomes, we propose a bold and transformative approach to healthcare professions education (Table 1). Adoption of this approach clearly requires the full engagement of institution leadership to accelerate the adoption of an interprofessional, experiential and performance-based model of education. The implication is that funding is required to provide safe and shared simulated environments in which to collaborate interprofessionally. Other compelling reasons for the investment in an interprofessional (IPE) approach to training include the changing learning styles of a new generation of digital learners, a venue to test and try new clinical processes and procedures, stimulate new research opportunities – especially in the human performance sciences, as well as help address the challenges of recruitment and retention of students and healthcare professionals.

| An interprofessional, experiential, performance-based approach to advancing IPE (iEXCEL) | |
|---|---|
| Challenges | iEXCEL solutions |
| Leadership | • Elicit strong leadership support from academic, community and clinical leaders – with patient safety, as well as healthcare professional wellness and safety – as driving factors. |
| Culture | • Ensure Deans and key administrators understand and ‘buy-in’ to the value of IPE as it relates to patient and staff safety. • Establish IPE as an institutional priority and highly valued educational experience by providing experiential, interprofessional activities. • Foster innovation in the learning and teaching environments. • Nurture and support student IPE, interest groups. • Include DEI and ‘wellness’ as key cultural necessities. |
| Logistical | • Creates shared interprofessional space where no one discipline ‘owns’ the space. The ideal space is a shared simulation centre with advanced technology so that students can learn to work in teams through simulated (real-life) activities. • Provide support to faculty as they adopt experiential learning using simulation and visualization. |
| Curriculum | • Develop an interdisciplinary IPE curriculum committee, with the role of chair – or co-chairs, rotating between healthcare disciplines. • Select faculty based on their passion for patient safety and innovative spirit. • Move to a small group IPE model. • Measure and assess the impact of IPE activities and elicit open feedback that gets shared with the curriculum committee. • Include students and listen carefully to their input. • Incorporate independent learning opportunities. • Count IPE experiences that are not embedded in the IPE ‘curriculum proper’ – as long as they meet predetermined criteria. • IPE curriculum should be longitudinal and for all levels of learning. |
| Use of New Technologies | • Introduce new educational technologies and software, especially simulation and visualization. • Consider shared investments in technologies, such as interactive digital walls. • Use a case-based approach to experiential and interactive learning. • Consider the needs of students working remotely. They, too, can be assigned to interprofessional groups and given projects. |
| Faculty Engagement | • Recognize and reward faculty and support staff who promote and support IPE and the activities and are recognized by students. • Identify IPE Awards – for curriculum innovation in IPE. • Provide seed funding to support IPE projects and outcome studies. • Encourage and help create an ‘Academy of Interprofessional Educators’ or similar groups to foster collaboration between faculty. • Foster innovation in educational and human factors research. |
While adopting an interprofessional and experiential approach to health professions education can provide the public with extra assurance that each trainee meets defined professional, procedural and team competencies, achieving a paradigm shift to a true interprofessional, experiential performance-based model can be challenging. This requires total ‘buy-in’ from institutional leaders, as well as commitment from the College Deans. Ideally, this requires creating shared experiential learning and simulation spaces that can accommodate team training. While the latter recommendation at first seems costly, there are, in fact, great efficiencies to be found when sharing space and simulation equipment, as well as being cost-effective related to embracing advanced technologies and software.
To be successful, a major paradigm shift in the education of health professionals must overtly, at its very core, address the safety and quality of care through the transitions from novice learner to mastery of skills for each specific discipline. The goal is to graduate healthcare professionals who are safe to diagnose, formulate care plans, function effectively in teams and practice proficiently in their professional arena, as discussed in this essay. Future clinicians must be both confident and competent in all defined core competencies and, especially, in safely conducting procedures that are required to practice within a specific discipline and functioning in highly effective healthcare teams.
We acknowledge Priscila Rodrigues Armijo, MD, for her work as a contributing editor who critically revised the manuscript for intellectual content.
None.
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.
None.
Not applicable.
The authors have no competing interests to declare relevant to this article’s content.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.