
With increased buy in for simulation education in regional areas, simulation services face unprecedented demand for education that outstrips staffing or financial capacity. Delivering simulation to regional areas comes with significant costs including equipment purchases, clinical coverage and travel costs. Faced with such obstacles, educators may be forced to offer education in insufficient doses or with excessive class sizes.
Innovations to mitigate the cost of delivering simulation remotely, include virtual simulation training and tele-debriefing [1,2]; however, simulation software and video calls come with their own challenges and don’t necessarily replicate work as done.
With an extensive geographical area, a large tertiary neonatal unit and five peripheral hospitals, our neonatal resuscitation Program Coordinator had a challenging remit. Our challenge was to find a new vector for course delivery that covered three key elements: small groups of participants, conducted at convenient times in their own hospital, with reduced travel for faculty.
We identified clinical equipment used in real resuscitations as an alternative technology for simulation delivery. In this paper, we describe the unexpected benefits of utilizing the telehealth device for delivery of our neonatal resuscitation programme, highlighting costs saved and the symbiotic advantages of utilizing tools designed for remote health care.
Fortuitously, a telehealth device was purchased in the birth suites of two of the peripheral hospitals to aid clinical staff in neonatal resuscitation. Staff identify when they require resuscitation assistance and press the emergency button which is connected to a tertiary centre Neonatal Consultant’s phone. Instant audio and visual connection between the tertiary centre and their peripheral unit via the tele-health device is provided. This allows assistance in real time during a resuscitation. Due to the low frequency of neonatal resuscitation in our regional sites, these devices are infrequently used allowing ample time for simulation. An adapted neonatal resuscitation program was created for a tele-simulation platform [3–5], and a course resource package sent to each of the hospitals.
The device provides two-way connectivity through an App on the computer in the tertiary centre, and a computer on wheels in the peripheral centre. There are also two cameras, one on the monitor and one on a boom. See Figure 1.

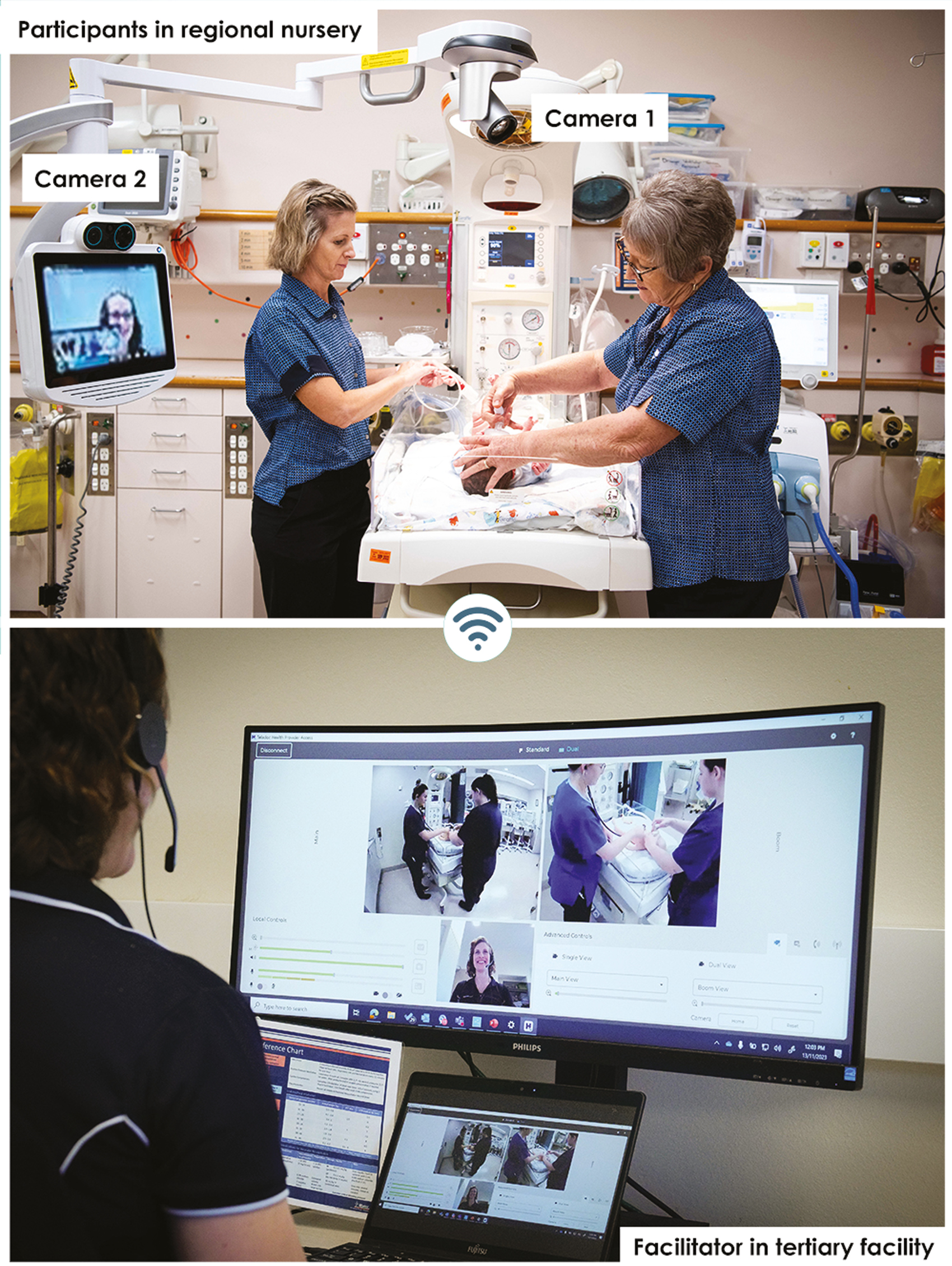
The dual-purpose telehealth/tele simulation platform and faculty terminal.
This provides the facilitator with full control of cameras to zoom in and out as well as 170 degrees pan rotational angle of the boom camera. Participants can see and interact with the tertiary centre support person on their screen whilst the faculty’s terminal displays both camera views on a split screen with complete control of the participants view.
Course evaluations showed comparable results with training conducted via face-to-face sessions, with increased confidence levels and comfort with simulation via tele-simulation. Verbal feedback confirmed an approachable and non-threatening technique. An unintended positive outcome was staff reporting increased familiarity with the device for clinical and educational use. This increased familiarity has germinated two new training programmes with the maternity and neonatal units now conducting fortnightly simulation and monthly clinical skills stations.
Participant dissatisfaction was a concern when switching to a remotely delivered course; however, the change yielded unanticipated benefits. The use of technology used in clinical escalation reinforced supportive relationships between regional and tertiary staff. Simulated resuscitation using the telehealth device improved psychomotor familiarity with infrequently utilised equipment. The virtual format forced a shorter course length, leading to decreased clinical impact on staffing. Once comfortable with the technology, regional educators began conducting more internal simulations.
We additionally compared the financial impact of conducting face-to-face simulation education vs remote training via the telehealth device. Table 1 details the analysis.

| Costs | Face to face inputs | Tele-simulation inputs | Savings via tele-simulation versus face to face |
|---|---|---|---|
| Telehealth unit | $0.00 | $0.00 | $0.00 |
| Attendees salary | 16 staff in two days (8hrs/day) | 16 staff in 4 days (4.5hrs/day) | $4400.00 |
| Faculty salary | 1 Neonatal Doctor 1 Clinical Facilitator |
Education Coordinator | $2580.00 |
| Travel Accommodation Food |
1 Neonatal Doctor 1 Clinical Facilitator |
$0.00 | $2700.00 |
| Total | $9680.72 | ||
| ROI = Benefits – Costs/Costs × 100. | 150% = $1.50 back on every $1 spent on training. |
Whilst this device cannot be moved from its clinical location, it has empowered the consideration of ‘dual-use-devices’ for both clinical guidance and education. The cost savings help mitigate the expense of the clinical purchase and an argument to fund the same devices for other departments is substantive.
The technology facilitates experiential learning, critical thinking, and decision-making in a risk-free environment to patients. Furthermore, our use of tele-simulation encourages collaboration among learners and experts across the state, enabling the exchange of knowledge and best practices. In this case scenario we have hijacked telehealth technology to provide training for neonatal resuscitation in remote locations resulting in evaluations comparable to face to face training, eliminating travel for faculty and participants, increasing staff familiarity with essential healthcare equipment, and creating an environment where staff want to train more regularly. This process could be extended to other departments that use telehealth technology. The authors recommend further research with other medical specialities, assessment of learning outcomes, and further exploration of clinician readiness using this model.
All authors contributed to project conception, design, and implementation. The authors jointly prepared the manuscript.
No funding was received for this project.
Not applicable.
Not applicable.
The authors declare no relevant conflicts of interest.
1.
2.
3.
4.
5.