
Simulation for non-pedagogical purposes has begun to emerge. Examples include quality improvement initiatives, testing and evaluating of new interventions, the co-designing of new models of care, the exploration of human and organizational behaviour, comparing of different sectors and the identification of latent safety threats. However, the literature related to these types of simulation is scattered across different disciplines and has many different associated terms, thus making it difficult to advance the field in both recognition and understanding. This paper, therefore, aims to enhance and formalize this growing field by generating a clear set of terms and definitions through a concept taxonomy of the literature.
Due to the lack of alignment in terminology, a combination of pearl growing, snowballing and citation searching approach was taken. The search was conducted between November 2020 and March 2023. Data were extracted and coded from the included papers according to seven Simulation-Based I’s (SBIs; Innovation, Improvement, Intervention, Involvement, Identification, Inclusion and Influence).
Eighty-three papers were identified from around the world, published from 2008 to 2023. Just over half were published in healthcare simulation journals. There were 68 different terms used to describe this form of simulation. Papers were categorized according to a primary and secondary Simulation-Based ‘I’. The most common primary SBI was Simulation-Based Identification. Selected categorized papers formed a descriptive narrative for each SBI.
This review and taxonomy has revealed the breadth of an emerging and distinct field within healthcare simulation. It has identified the rate at which this field is growing, and how widespread it is geographically. It has highlighted confusion in terminology used to describe it, as well as a lack of consistency in how it is presented throughout the literature. This taxonomy has created a grounding and step change for this work which is embedded in the literature, providing a rich and varied resource of how it is being utilized globally.
What this study adds
• A literature-based identification of an emerging area of healthcare simulation.
• A concept taxonomy with examples from around the world.
• A descriptive narrative of each Simulation-Based ‘I’.
• Recommendations for future work within the field.
Simulation as a tool for non-pedagogical purposes has begun to emerge over the past decade; however, its objectives and design are often confused with simulation-based education methods, or focused on individual institutions’ needs and uses that have developed organically. There is, therefore, a gap in the literature in terms of a common understanding in how this is defined, described and conducted. With more and more papers emerging, more terms and possible applications being generated, confusion is mounting and no one approach captures all that it does and could encompass. It is, therefore, imperative that this new and exciting development within healthcare simulation has a guiding framework that the simulation community can adopt and evolve. Drawing on the growing global literature to do this is the fairest and most logical approach, as it recognizes the breadth of work that has already been conducted and does not favour one approach. However, this approach is not definitive and will ultimately require further development and refinement by those in the field as further knowledge and understanding develops.
Although slow to get started from a practice and research perspective, the concept of simulation for non-pedagogical purposes is not new and in fact was predicated by Gaba almost 20 years ago [1, p.i2] when he stated his ‘vision of how fully integrating simulation into the structures and processes of healthcare can be used to revolutionize patient care and patient safety; and to provide an overview of the driving forces and implementation mechanisms by which different entities may, or may not, promulgate simulation over the next 20 years’. We are now seeing that it is increasingly used for the study of systems, quality improvement initiatives, testing and evaluating of new interventions, policies and procedures, co-designing new models of care, exploring human and organizational behaviour, workforce development, comparing different sectors, and identifying system glitches, safety threats and misunderstandings, with consequent benefits for a more safety focussed, lateral thinking and cohesive workforce [2–8].
Additionally, national bodies are recognizing the opportunities of this shift in focus. For example, England’s Health Education body (Health Education England) has developed a strategic vision that identifies simulation to support ‘key national policy and strategic developments that are influencing the current and future workforce requirements across the health and care system’ [9]. They term this use of simulation as ‘simulation-based interventions’ and describe a few case studies where this has been achieved. In addition, they stipulate key national policies that experienced commentators believe ‘effective simulation-based interventions’ could support. They describe the application of simulation as a tool to address system-wide challenges that are being faced by health and care providers, including supporting workforce transformation as part of the process of system redesign, and to support key national policies and strategic developments. However, they stop short of clearly categorizing and describing how simulation of this type can be designed, delivered, translated into practice and reported. Although comprehensive and refreshingly forward-thinking in its vision, and providing a good foundation upon which to develop this growing area, it lacks the bigger picture across all these forms of simulation, and their potential applications and affordances. From another angle, the Health Quality Council of Alberta [10] in Canada have provided evaluation simulation guidelines to optimize the return on investment when evaluating healthcare facility designs for quality and patient safety. They state that ‘conducting simulation-based evaluations (regardless of the type) is perceived by non-participant stakeholders to produce findings that are useful for future projects. Moreover, the process engaged end-users to the extent that they felt they were able to effectively evaluate the design of the room and make meaningful contributions to improve the design’. Although specific guidance is provided, it is not sufficiently generic to be of universal value.
Ultimately, this growing body of work and area of interest need an umbrella term and clear specific definitions to guide and develop the field both in practice and research. Therefore, the authors of this paper have coined the term ‘transformative simulation’ to describe simulation as a tool to transform health and care through collective understanding, insight and learning, and to distinguish it from the more traditional educational/pedagogical approaches that are more commonly practised, or from specific system-focussed applications only. This is an important step-change within the field as it aims to provide clarity within a complex area that is at risk of not advancing in quality and structure due to the ad hoc and opportunistic approach that is often taken due to a lack of a guiding framework. There is also a more serious issue at stake in that simulation conducted of this type without a recognition of what it is ultimately trying to achieve, risks unearthing issues that are not able to be addressed which could generate ethical dilemmas for those with good intentions.
This paper, therefore, aims to enhance and formalize the growing field of ‘transformative’ types of simulation by reviewing the existing literature and drawing on the authors’ extensive experience in this area, their networks, and engagement within the wider simulation community, to provide a more comprehensive understanding of the field, its application, utility and gaps. In addition, it aims to generate clear terms and definitions that the simulation community can use for clarity and purpose – ultimately developing a framework from which advancements can be made to the benefit of all.
The principal issue in developing this use of simulation, both in recognition, understanding and advancement, is that the literature related to these types of simulation activities is scattered across different disciplines and typically focuses on a single aspect of the simulation activity under study. For example, as simulation of this sort spans organizational, policy, engagement and patient safety fields, it can be found in any of these associated journals and more. Additionally, because there is no defined terminology, descriptions and terminology used are diverse and reflect meeting publication criteria as much, if not more than, outcomes. It is, therefore, impossible to draw on traditional literature-reviewing methods and instead a pearl growing, snowballing review of the literature approach was taken to generate a taxonomy of what this non-pedagogical form of simulation encompasses. This approach is not only the most pragmatic way to pursue this aim but it is anticipated that the resulting taxonomy will provide an evidenced-based framework and coherent terminology that future authors can draw on to situate their work for appropriate recognition.
In its basic definition, a taxonomy is a structured set of names and descriptions used to organize information and documents in a consistent way [11]. A ‘knowledge taxonomy’, focuses on enabling the efficient retrieval and sharing of knowledge, information and data across a discipline by building the taxonomy around the knowledge need in an intuitive structure [11,12]. Taxonomies are crucial for the management of complex issues. Pincher [13] argues that, without a taxonomy designed for categorization and management, or one that supports better searching, understanding and clarification can be lost.
Taxonomies can contribute to making explicit knowledge embedded in the literature by mapping and categorizing tacit knowledge embedded in existing expertise. They promote collaboration and sharing between individuals and groups by mapping and coordinating the collegiate enterprise [11,12]. Taxonomies help putting knowledge into practice by making sense of the knowledge of the subject and creating a common vocabulary and a common way of working. They have, therefore, to be treated as an essential part of the knowledge management strategy of an emerging field to ensure appropriate advancement [13].
Between November 2019 and March 2020 and based on the available literature at the time, Weldon (SW) identified categories relating to five specific objectives/focuses that became apparent from reviewing the literature. After the COVID-19 pandemic hit, it became apparent that there was an increase in publications related to this type of simulation and Weldon (SW) subsequently engaged with Buttery (AB), Spearpoint (KS) and Kneebone (RK) to develop the field and understand it further. This resulted in meetings with stakeholders (different healthcare professionals conducting transformative types of simulation within healthcare organizations in the UK), Twitter Fests (pre-set and advertised dates and times via a simulation society for a discussion on a topic via a series of questions), and workshops with the simulation community through communities of practice (healthcare simulation conferences and networking events) and an international simulation society (Association for Simulation Practice in Healthcare – ASPiH). In addition, a Specialist Interest Group (SIG) was set up in 2021 via ASPiH that was accessible to members and non-members. This 2-year consultation with the simulation community resulted in a further two categorizations making seven categories under the umbrella term of ‘transformative simulation’, this created a Simulation-Based ‘I’ (SBI) rainbow (Figure 1). There was also further recognition that most forms of transformative simulation activities met more than one category (Table 1). With this clearer understanding, the authors conducted a literature search during July 2021.

| Innovation | Introduction of novelties; the alteration of what is established. |
|---|---|
| Improvement | Making something better; becoming better; an addition or alteration to make a change for the better. |
| Intervention | The action of intervening or interfering in any affair to affect its course or issue. |
| Involvement | The process of involving; being involved; being implicated, entangled or engaged. |
| Identification | The act of identifying; what or who; discovery and recognition. |
| Inclusion | The action or an act of including something or someone; the fact or condition of being included. |
| Influence | To exert influence; to work influentially on, upon person(s) or thing. |


SBI rainbow.
A combination of ‘pearl growing’ (using potentially relevant search terms/keywords to identify associated literature), ‘snowballing’ (tracking down relevant references in key papers), and citation searching (identifying who has cited a relevant paper since its publication and checking to see if it is relevant) approach was taken [14]. The authors’ own awareness, networks and memberships were also utilised.
Due to the unconventional approach required for this type of review, searches informally commenced in May 2017 once the change in application was identified as beginning to emerge as a field. By November 2020, due to the COVID-19 pandemic and a recognized increase in the literature being published on this subject, the search strategy was formally commenced (November 2020–March 2023). Drawing on literature identified and filed between 2017 and 2020, potentially relevant terms/keywords were identified and used for further searches. Searches of the following databases was conducted: Scopus, Medline, PsycInfo and CINAHL. Followed by pearl growing, snowballing and citation searching. When new papers were identified, the process began again until no further papers were identified (Figure 2).

Search process.
All papers that described the use of health and social care simulation beyond a pedagogical structure (such as skills acquisition and assessment), even if this was also described, were included. No date, country or language restrictions were applied; however, literature reviews, opinion pieces and editorials were excluded, as they did not provide primary evidence of the approaches direct use or consideration.
Data from all identified papers were extracted into an Excel spreadsheet. Categories for extraction included journal, publication type, location, simulation type/definition, simulation study/description, objectives and goals, target participants, outcomes, impact, terms used to describe the simulation activity, other relevant terms, primary SBI, and secondary SBI.
Weldon (SW) then coded each category according to the definitions related to each SBI, generating primary and secondary SBIs for each paper. Spearpoint (KS) and Buttery (AB) then checked the categorization according to the definitions, and discussions were held where a consensus was not agreed. This process enabled the preliminary categories to be tested whilst identifying if there were any categories missing or where categories could be combined/added.
As this is a taxonomy, the information extracted from the studies included was in relation to the type of transformative simulation being presented and not any evaluative or research methods as it is beyond the scope of this paper to assess each type. Rather our aim was to combine and categorize. Information relating to publication/study type was extracted to generate an overview of how the data are communicated in the literature and to identify gaps in the research so that recommendations for future advancement for the field can be made.
Eighty-three papers were identified and included in this review with a publication date range from 2008 to 2023 (Supplement 1). Thirty-one papers were excluded after a detailed review revealed they did not meet the inclusion criteria (Supplement 2 provides the excluded papers and their reason for rejection). Figure 3 illustrates the increasing rate of publications on this type of simulation year by year. Twenty-six were from the UK, 22 from the USA, 16 from Canada, 6 from Australia, 4 from Denmark, 2 from Spain, 1 from Qatar, 1 from Lebanon, 1 from Brazil, 3 were multi-country (Australia and Canada; Norway, Denmark and UK; Hong Kong and UK), and 1 was unknown. Just over half the publications (42) were published in simulation-specific journals (International Journal of Healthcare Simulation (IJoHS); Simulation in Healthcare; Advances in Simulation; BMJ Simulation & Technology Enhanced Learning (STEL); Clinical Simulation in Nursing), the remaining were published in a mixture of specialist and general medicine (14), quality and patient safety (10), environment research and design (4), education (5), health services and management (2), communication (2), history (2), military (1), and science (1) journals.

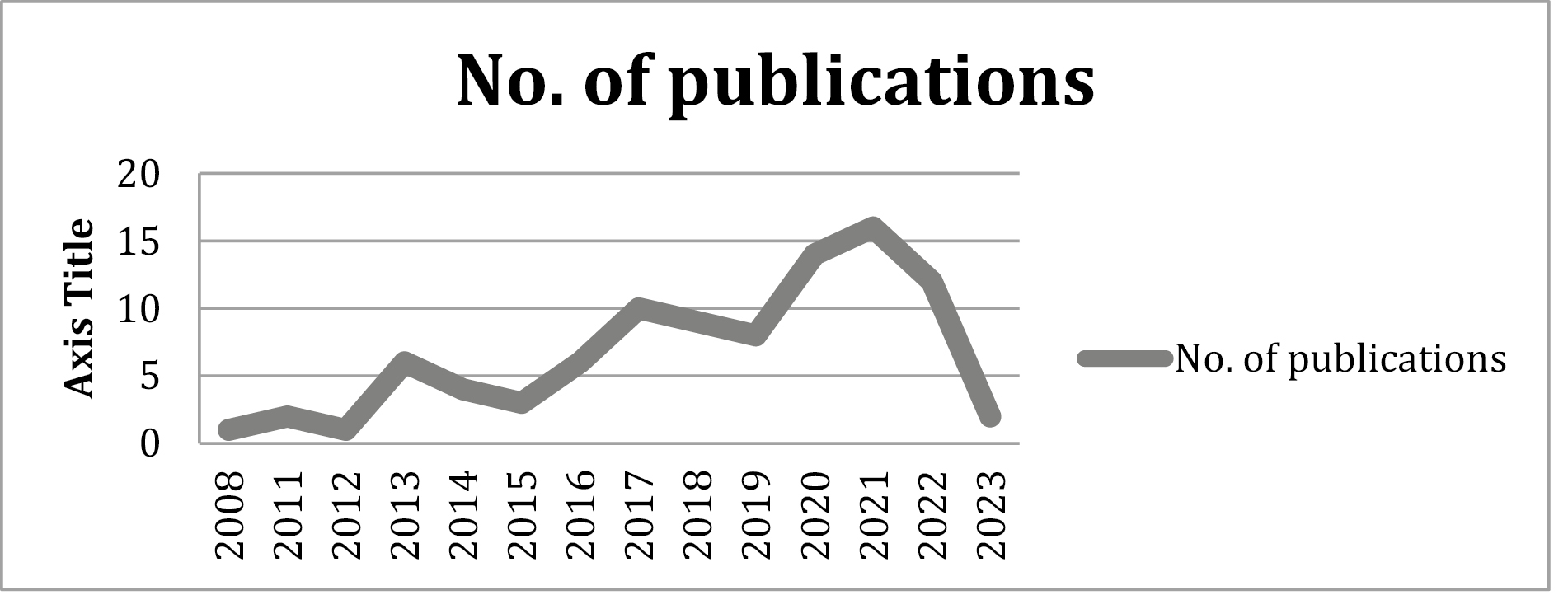
Number of publications per year.
Across the papers, 68 different terms were used to describe the simulation activity (Table 2). The terms used appeared to focus on different aspects of simulation, for example, some were described by the location (e.g. in situ simulation), or the ‘realism’ of the simulation (e.g. high-fidelity simulation). Others focused on what the simulation was about (e.g. clinical or system focused). Some were more related to the design (e.g. sequential simulation), and others the participants (e.g. multidisciplinary simulation). This highlights the many ways simulation can be described, not just for transformative forms but also more generally too, and thus the need for a universal taxonomy.

| Terminology used | No. of times used |
|---|---|
| Location/contextual/realism focused | |
| In situ simulation | 26 |
| In situ simulation training | 1 |
| Immersive full-environment in situ simulation | 1 |
| Immersive realistic in situ simulation | 1 |
| Immersive simulation | 2 |
| Inter-professional in situ simulation | 1 |
| On-site simulation | 1 |
| Centre-based simulation | 1 |
| High-fidelity simulation | 3 |
| Design/resource focused | |
| Sequential simulation | 6 |
| Distributed simulation | 7 |
| Simulation-based user-centred design | 1 |
| Tabletop simulation | 2 |
| Clinical simulation scenario | 1 |
| Technology-enhanced simulation | 1 |
| Outcome focused | |
| Translational simulation | 3 |
| Simulation-based research | 1 |
| Simulation-based intervention | 1 |
| Participant focused | |
| Simulation-based inter-professional education | 1 |
| Multidisciplinary simulation | 1 |
| Behavioural simulation | 2 |
| Participatory behavioural simulation | 1 |
| Simulation with standardized patients | 1 |
| System focused | |
| Process-orientated simulation | 1 |
| System integration simulation | 1 |
| Simulation for systems integration | 1 |
| Patient safety and system integration simulation | 1 |
| System-focused simulation | 2 |
| System-focused simulation-based approach | 1 |
| System-based investigation | 1 |
| System-based clinical systems testing | 2 |
| Simulation-based systems testing | 1 |
| Macro-systems simulation | 1 |
| Simulation-based quality improvement observation tool design | 1 |
| Systems-based in situ simulation | 1 |
| The patient environment simulation for systems integration | 1 |
| Code silver exercise/in situ CSE/virtual CSE | 1 |
| Simulated complex systems | 1 |
| Simulation-based intervention | 1 |
| Clinical focused | |
| Trauma simulation | 1 |
| Simulated inter-operative clinical contexts | 1 |
| Engagement focused | |
| Immersive engagement | 1 |
| Engagement through simulation | 2 |
| Simulation-based engagement | 1 |
| Generic | |
| Simulation | 11 |
| Live simulation | 1 |
| Live medical simulation | 1 |
| Simulation-based mock-up | 2 |
| Simulation-based training | 2 |
| Simulation training | 1 |
| Simulation-based enactment | 1 |
| Simulation-based re-enactment | 1 |
| Scenario-based simulation | 1 |
| Simulation-based activities | 1 |
| Simulation-based techniques | 1 |
| Other | |
| Simulation health economy | 1 |
| La-based simulation | 1 |
| Lateral play | 1 |
Publication types were highly varied and ranged from case studies, reflections and evaluations, to research, theoretical papers, frameworks and ‘how-to’ strategies. Due to the complexity of these types of simulation, the many potential areas of focus, and a lack of an umbrella term and guiding framework, the papers’ objectives and focus were also highly varied and frequently lacked clarity in expressing ultimate purpose, often with several goals and objectives intertwined but not clearly defined. This meant that extracting data on the papers’ goals and objectives for the use of categorization required careful analysis of the paper to identify what they were – and, where there were multiple objectives, which were pertinent to transformative forms of simulation. There was also confusion in the reporting which we contend is due to trying to fit transformative types of simulation into a simulation-based education pedagogic reporting framework, further reflecting the need for clarification.
The literature reviewed by Weldon, Buttery and Spearpoint was categorized according to the below seven SBIs. However, many papers’ objectives and goals reflected more than one SBI and therefore they were further categorized to reflect primary and secondary objectives (Supplement 1).
All SBIs were utilized, the most common SBI used overall was identification (38), the frequency of primary objective alone was identification (26), followed by then influence (14), improvement (13), involvement (12), inclusion (7), intervention (5) and innovation (4). No further SBIs were identified from this review (Table 3).

| SBI | Primary objective | Secondary objective |
|---|---|---|
| Innovation | 4 | 3 |
| Improvement | 13 | 20 |
| Intervention | 7 | 5 |
| Involvement | 12 | 1 |
| Identification | 26 | 12 |
| Inclusion | 7 | 5 |
| Influence | 14 | 7 |
The following narrative provides examples of some of the included papers’ objectives and outcomes of the studies categorized to each SBI. Although many studies had primary and secondary SBIs, this narrative focuses purely on the primary objective and has therefore excluded objectives that have been defined as secondary. This is not to detract from transformative forms of simulation having more than one objective but to ensure clarity at this early stage of understanding. This develops the transformative simulation categories from a dictionary definition (before the review and taxonomy) to a data- and community-driven definition, and helps to build a picture of how each category is being employed in practice as well as its potential.
The Simulation-Based Innovation category is concerned with the introduction of something new or a new way of doing things. As an example, Blanks [21] used an innovation approach to evaluate the efficacy of simulation-based techniques to assess developing polices prior to implementation. They found that using simulation in this way enabled for the safe evaluation of new policies before publication to ensure they are appropriate for front-line use. Alternatively, Madani [44] explored the role of simulation as a potential testbed for diminishing the risks, pitfalls and resource demands associated with the development and implementation of medical innovations, and more specifically the product development pathway. They found that simulation had the strongest role for early prototyping, testing for safety and product quality, and testing for product effectiveness and ergonomics.
The Simulation-Based Improvement category is concerned with using simulation to make something that already exists better and in line with best practice. In their cohort study, Whitfill [18] aimed to compare the US National Paediatric Readiness Project score before and after an in situ simulation-based quality improvement programme across Connecticut hospitals. They concluded that participation in a simulation-based quality improvement collaborative was associated with improvements in paediatric readiness. Similarly, Rojo [39] used simulation to understand care processes reorganization to improve efficiency whilst maintaining patient safety. They concluded that simulation could promote and facilitate change in patient care and organizational re-engineering.
The Simulation-Based Intervention category is concerned with changing a situation or way of doing things. In their paper, Dube [42] described the implementation of a central simulation COVID-19 response team by integrating new components such as novel workflows, protocols and cognitive aids, with rapid changes to practice and care delivery. They concluded that the programme was highly coordinated and enabled sharing across the largest single health authority in Canada.
The Simulation-Based Involvement category is concerned with inviting and engaging otherwise excluded individuals or groups with the purpose of generating new experience and perspectives and to ultimately bridge understandings. In their qualitative study, Korkiakangas [6] used simulation based on prior observations to enable the general public to experience a re-creation of care in the dining and healthcare sectors, followed by discussions of the experiences. Using simulation, they were able to focus on the relational moments of care, unpacking the differences and similarities between dining and clinical care, and asking what participants liked or disliked in the simulated environments. Resulting themes indicated how the simulation participants felt about the care they received in real time and provided recommendations for improved clinical practice. They concluded that simulation provides a new kind of opportunity to bring professionals and patients together for focused discussions, prompted by immersive experiences of care and communication. Weldon [50] used simulation as a tool to engage future healthcare managers in the complexities of redesigning a care pathway process giving particular consideration to local initiatives and cost implications. The approach demonstrated that simulation has wider potential and can be particularly useful in the bringing together of many minds to speak the same language. Similarly, Pillay [73] developed a simulation that focussed on a non-hierarchical, equal partnership between neonatal teams from different unit designations. They concluded that the simulation was an acceptable method of promoting multidirectional understanding within neonatal teams of differing designations.
The Simulation-Based Identification category is concerned with the use of simulation to identify, discover or recognize what is happening in a given situation or set of circumstances. This is illustrated through Adler [8] who describes the use of simulation as a method to test systems to identify and reduce latent safety threats present at the opening of a new hospital. They concluded that approximately 641 unique issues were identified through the use of simulation prior to the hospital opening. A similar approach was taken by Colman [53] when opening an outpatient subspecialty clinic and with similar outcomes, and Jafri [78] for recommendations on safety checks before initiating a new programme.
Nielsen [56] explored whether higher numbers of failure modes, causes and effects, in a healthcare process, could be identified when a group of process experts actively simulate the process, as compared with brainstorming on this question. They concluded that the use of simulation enhanced a traditional healthcare failure mode and effects analysis.
The Simulation-Based Inclusion category is concerned with including key stakeholders to share, empower and enable. For example, Weldon [4], in their mixed-methods study, used simulation to inform, design and operationalize integrated care within health jurisdictions from a ‘bottom-up’ approach in order to fully engage and involve all stakeholders. They concluded that the systematic data collection from the diverse ideas generated through the simulation facilitated a much-needed ‘ear’ to those providing the solutions, as well as a legitimate and balanced perspective. Geis [33] used simulation for an investigative pilot with a range of objectives including defining optimal healthcare team roles and responsibilities, and refining the scope of practice of healthcare professionals. The simulations revealed the need to modify provider responsibilities by demonstrating that the medication nurse had the greatest workload during resuscitations and modifying medication delivery was deemed critical.
The Simulation-Based Influence category is concerned with exerting influence on someone or something. In their qualitative study, Brazil [58] used simulation to understand how an established trauma simulation programme was perceived by trauma care providers to influence their relationships with others and to identify those aspects of the simulation experience contributing to relational outcomes. Their findings suggested that simulation can have a profound influence on the relational aspects of care and the development of a collaborative culture, with perceived tangible impacts on teamwork behaviours and institutional systems and processes.
In their mixed-methods study, Weldon [49] designed a simulation of a series of short scenes built up from a collection of real patient healthcare journeys to illustrate to GP receptionists the importance of their role within the patients’ journey and influence how they practised. The simulations were designed to highlight the consequences of disjointed care, aiming to show that individuals in the pathway often act in silos, focusing on their own short interaction, without understanding the impacts of their action throughout the care pathway. In 2013, Tang [46] set out to ‘heighten students’ aspirations in medical science by using simulation to give the taste and feel of what it could be like for them’. They believe this approach has major potential for making the closed world of surgery accessible to young people who are considering a career in health care.
This literature review has revealed that transformative forms of simulation have been embraced and implemented successfully, for a range of reasons, globally over the past 14 years. In the UK, examples of its use include to investigate, understand and improve management and policy-making in a healthcare organization, inform, design and operationalize integrated care from a bottom-up approach to engage, identify, compare and contrast the experience of care in a day surgery unit, and encourage primary, secondary and tertiary services to function in a more integrated fashion to name but a few [3,4,6,24].
In Canada and the USA, transformative simulation has been used to test the opening of a new healthcare facility by identifying latent safety threats, and screening for unintended consequences of proposed solutions, as well as testing the systems and preparing staff for the transition to a new hospital [2,7,8,34,38]. In the USA, Norway, Denmark, Lebanon and Australia, it has been used to define optimal healthcare team roles and responsibilities, and refine their scope of practice [5,34], and as a response to different elements of the COVID-19 pandemic [16,23, 28,31].
Although varied examples of transformative simulations exist globally, there is little in the way of robust guidance or models that goes beyond specific applications within individual organizations. In Australia, Brazil [66] described their organization-wide simulation strategy development. They used the COVID-19 pandemic as an example where they were able to deliver more than 250 translational simulations, involving more than 1500 healthcare staff, across multiple hospital departments within a 30-day period (March 2020). Barlow [7] has developed a documentation framework for ‘simulation quality improvement activities’ that evaluate patient care workflows, processes and systems, to capture and report findings of system deficits identified in the simulations to key decision-makers. In Canada, it has been used province wide as a first choice strategy for ensuring individual, team and system readiness of the pandemic. In their paper, Brydges [31] conclude that ‘the pandemic cemented simulation as fundamental for any healthcare organization interested in ensuring its workforce can adapt in times of crisis’. Given the likelihood of the ongoing need for healthcare change post-COVID-19, transformative simulation approaches will remain critical and, therefore, this field has the potential to advance exponentially with the required guidance and evidence in place.
Although implementation of transformative simulation is clearly taking place, few organizations have recognized or incorporated it as a tool into their normal practice. In many organizations, it is common for impassioned practitioners to carry out transformative simulation activities in their own time using existing resources. This involves drawing on simulation-based education resources, then using the outputs to convince their organization of the value of the approach whilst trying to secure more resources to make it sustainable. This undermines the organizations’ ability to fully capitalize on the benefits of transformative simulation. Furthermore, little implementation guidance is available. Only a few general frameworks to guide implementation efforts have been published, all of which are based on personal reflections rather than robust or varied research evidence [31,32,65]. It is, therefore, likely that they do not reflect the unique characteristics of all healthcare systems or capture the detail and flexibility required. In their review of the literature, Cohen [40] concluded most reports they reviewed neither described the simulation methodology in sufficient detail to determine its validity, nor was the process of analysis described sufficiently to be certain that conclusions were balanced and reflective of the proceedings. They stated that a clear description of a transparent, validated method and analysis framework, including triangulation of evidence and assessment scales, could provide reliable evidence upon which policy makers and stakeholders could act. In their commentary back in 2013, Salas [22] situate what is known about simulation in health care at the time, and predicted ‘critical future research and application directions for simulation as a patient safety strategy’ through the promotion, reinforcement and development of attitudes for effective patient care. They state that ‘new insights from neuroscience, organisational, cognitive, human factors and team sciences will help make simulation even more effective, creating a new world in which our imagination will be the limit’.
The presented taxonomy provides practitioners and researchers with an objective-driven description of transformative forms of simulation that enables a more robust, unified format and process. We believe that the current confusion across the literature, and the inability to advance this field beyond individual accounts, could be solved by situating it within this taxonomy of terms, definitions and examples. We would hope that through generating a shared understanding based on existing work conducted within the global simulation community over the past decade, more examples can be added generating further evidence that can be collectively examined, and universal design considerations and guidelines developed.
Due to the methods applied, we are unable to be confident in the comprehensiveness of the search; however, we hope that this pragmatic approach generates further clarity that can help to advance the field. Although no date or language barriers were applied to the search, we recognize that the methods (pearl growing, snowballing and citation searching) would likely not pick up many non-English written papers. As this field grows, we hope that the clarity being created will in time reveal a breadth of non-English written papers that can be added to the growing body of work and understanding.
Based on this review and taxonomy, we recommend that simulation practitioners aim to consider what their primary and secondary (where applicable) SBIs are when conducting transformative types of simulation – for design, outcome and reporting clarity. We suggest that researchers consider the different objectives and uses the taxonomy has described and pose the questions that need to be answered as well as developing the studies that can answer them. We encourage debate around the taxonomy and expect to see it evolve over time as the simulation community make use of this new platform to grapple with this powerful use of simulation that has huge untapped potential and impactful benefits for health care and simulation globally.
This review and taxonomy has revealed the breadth of an emerging and distinct field within healthcare simulation. It has identified the rate at which this field is growing, and how widespread it is geographically. It has highlighted confusion in terminology used to describe similar applications of this form of simulation as well as a lack of consistency in how it is presented throughout the literature. This taxonomy has created a grounding for this work which is embedded in the literature, providing a rich and varied resource of how it is being utilised globally. Just as Bloom’s taxonomy contains multiple terms under each level of complexity, transformative simulation is not absolute or constraining, but descriptive, supporting and evolving.
This paper aspires to create a step change in the understanding, employment and reporting of simulation for health and care, by generating a living, robust but evolving framework from which transformative forms of simulation can be situated, understood, developed and researched.
Supplementary data are available at The International Journal of Healthcare Simulation online.
None declared.
None declared.
Through corresponding author.
Not required.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
83.
84.
85.
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.
102.
103.
104.
105.
106.
107.
108.
109.
110.
111.
112.
113.
114.
115.
116.