
We investigated the impact of a health sciences centre-wide, high-fidelity, simulation-based interprofessional team training program on participants’ knowledge, skills and attitudes towards teams and teamwork.
Senior medical, nurse anaesthesia and allied health profession students participated in dual-scenario, simulation-based, interprofessional team training sessions with immediate debriefings about team-based competencies (2015–2017). Pre- and post-intervention, students completed the Interprofessional Teamwork (IPT) questionnaire and the Readiness for Interprofessional Learning Scale (RIPLS). Observers and students rated team performance using the Teamwork Assessment Scales (TAS). Descriptive statistics were determined for IPT and RIPLS items and TAS subscales; student t-test or one-way ANOVA compared scores. Medical students completed the TeamSTEPPS™ Teamwork Attitudes Questionnaire (T-TAQ) at the beginning and end of senior year. Matched mean scores were calculated for T-TAQ subscales; paired t-tests and linear regression compared annual scores within and between years and, in 2015, trained and non-trained students.
Students from five health professions participated (n = 659). Significant improvements occurred in matched scores across all 3 years for every IPT item and most RIPLS items. Significant improvements occurred annually for each matched observer-, peer- and self-rated TAS subscale score across scenarios. Significant changes in matched T-TAQ subscales included a decrease in mutual support in non-trained students in 2015 and an increase in situation monitoring for 2017 students. Between years, significant changes in matched T-TAQ subscales included an increase in leadership (2015–2017) and situation monitoring (2016–2017).
A health sciences centre-wide high-fidelity, simulation-based, interprofessional team training program improves students’ team-based behaviours, teamwork attitudes and interprofessional learning attitudes. Widespread adoption of such large-scale team training programs has the potential to improve teamwork among healthcare providers over time.
Teamwork is essential for delivering quality, safe care to patients in today’s complex healthcare environment. Many examples demonstrate its multi-tiered impact on patient care, staff morale and organizational function [1,2]. Among acute care teams, a positive, medium-sized correlation exists between teamwork and clinical performance [3]. A flattened hierarchy improves job satisfaction and decreases emotional burnout in the operating room (OR) [2]. Role confusion impedes the effectiveness of surgical teams [4]. Finally, ineffectual conflict management hinders team dynamics in the intensive care setting [5].
Unfortunately, ineffective teamwork tends to be the norm in healthcare [6]. Ingrained professional identities and hierarchical structures disconnect team members [4]. As a result, a silo mentality fosters tribalism in which one team profession attributes preconceived traits to another [7]. In addition to its deleterious impact on team function, such behaviour influences future performance through its pernicious effect on health professional students who begin to mimic it on clinical rotations [8]. This role modelling is an important social factor of the hidden curriculum for medical students [9] and undergraduate nursing students [10].
In an effort to break down these silos and counteract negative role modelling, educators have focused on integrating interprofessional education (IPE) into health sciences curricula. Bringing students from two or more professions together to learn with, from and about each other [11], IPE interventions have a positive impact on participants’ knowledge, skills and attitudes [12]. In addition, it is a particularly effective method for team training of pre-licensure students [13].
In both team training [14] and IPE [15] in healthcare, simulation-based approaches are popular modalities. Attractions of simulation-based training (SBT) include its immersive, experiential character and its ability to have students learn in a safe environment in which their actions do not pose any risk of harm to actual patients [16]. For health professional students, team-based SBT has beneficial effects in terms of insight related to deficiencies in team-based competencies [17] and a desire to conduct more IPE team training activities [18].
For more than a decade, the authors have incorporated small-scale, high-fidelity SBT of interprofessional student teams into curricula from the Schools of Medicine, Nursing, and Allied Health Professionals at our health sciences centre [16,19–21]. We wanted to investigate the impact of a health sciences centre-wide, multi-year team training program on learners’ acquisition of knowledge, skills and attitudes towards teams and teamwork [6]. We hypothesized that incorporating interprofessional team SBT into the curricula of medical, nursing and allied health professional students would improve such knowledge, skills and attitudes among participants.
We have published a detailed description of the methodology for this project previously [6,20]. The protocol involved a quasi-experimental design with prospective collection of pre-/post-intervention data. Institutional review board approval as an exempt study occurred prior to any data collection.
The Louisiana State University (LSU) Health New Orleans Health Sciences Center comprises six schools, including medicine, nursing, allied health professionals, dentistry, public health and graduate studies. All the schools except for dentistry are co-located on a campus near the central business district of New Orleans. From January 2015 to June 2017, health professional students and faculty from the Schools of Medicine, Nursing, and Allied Health Professionals participated and taught in the SBT sessions, whereas faculty and students from the School of Public Health assisted in the statistical data analysis.
Training sessions occurred at the LSU Health New Orleans School of Medicine Learning Center, a 30,000 square foot, two-floor simulation centre located on the campus of the LSU Health New Orleans Health Sciences Center. Simultaneous sessions occurred monthly on each floor in rooms dedicated to high-fidelity SBT. Each room had a full-scale, computer-operated human patient simulator (HPS) manikin (CAE, Inc., Montreal, Canada) that served as the scenario’s ‘patient’ who started the scenario on a ‘bed’ lying down. The ‘location’ of the patient room was either in the emergency department or in the intensive care unit, depending upon the SBT scenario. Teams had the necessary equipment available for each scenario.
At the start of each training setting, designated participants started within the patient room as the initial caregiver for the patient. The remaining participants were outside the patient room at a distance as caregivers in other locations within the department or intensive care unit available for assistance in the case of patient deterioration.
The training format followed prior ex cura [18–21] high-fidelity SBT interprofessional student team training curricula implemented by the authors and others at LSU Health New Orleans. In brief, each session began with a pre-brief by facilitators related to the SBT format, its objectives and ground rules. Following this pre-brief, participants completed a first scenario immediately followed by an after-action facilitator-guided structured debriefing focusing on a set of team-based competencies: shared mental model, situation awareness, cross monitoring, open communication, resource management, anticipatory response, flattened hierarchy, role clarity and mental rehearsal. It also included a review of clinical care and military veteran behavioural health issues commonly encountered by providers. Participants would then complete a different second scenario to practice learned lessons, followed by another immediate after-action facilitator-guided structured debriefing expanding on themes related to teamwork and applications to practice. The session then concluded with a summary that elicited a commitment from each participant to employ one of the team-based competencies in clinical practice.
Three faculty instructors typically led each session. One instructor would operate the computer-based manikin, and two instructors would serve as facilitators during the structured debriefing. At least two instructors, typically the facilitators, would serve as raters of team-based behaviours following each scenario/debriefing cycle. These facilitators adhered to established effective debriefing principles and techniques in order to promote optimal learning [22–24]. Video-review rating replaced immediate after-action rating in cases where only one rater was available to evaluate team performance during a session. If additional instructors were present, they served as raters.
All faculty instructors participated in a half-day faculty development initiative before serving as facilitators and raters for observer-based team performance. The course occurred annually at the beginning of the academic year in the month of August. It consisted of a 2-hour didactic session focusing on organizational culture and human factors in healthcare. Objectives of this session included comparing and contrasting error response in different organizational cultures, defining features of a culture of safety, discussing the role of human factors engineering in promoting safety and illustrating high reliability in team function and its application to and assessment in the OR. Following the didactic session, faculty then participated in a 2-hour interactive session in which they became familiar with the Teamwork Assessment Scales (TAS), the team assessment instrument for the program [19,20]. The TAS is an 11-item tool using a 6-point Likert-type scale (1 = Definitely No to 6 = Definitely Yes) divided into individual and overall team performance components. The individual component is a 5-item Team-Based Behaviour (TBB) subscale. The overall teamwork component has a 3-item Shared Mental Model (SMM) subscale and a 3-item Adaptive Communication and Response (ACR) subscale. After review of the TAS, the faculty then broke into small groups to undergo observer training. This training involved watching videos of team interactions, rating performance on the TAS and discussing scores in order to develop agreement on observed performances. In addition, faculty participated in a separate development initiative involving didactic instruction on common mental health challenges faced by military veterans and their recognition.

| IPT questionnaire itema | Total N | ∆ (post – pre)b | p- valuec, d | ||
|---|---|---|---|---|---|
| Range for all years | Year 1 (130 ≤ N ≤132) | Year 2 (N = 246) | Year 3 (249 ≤ N ≤ 251) | For each year | |
| Have a common understanding of patient’s condition. | 625–629 | 0.63 (0.94) | 0.76 (1.05) | 0.50 (0.91) | <0.001 |
| Have a common understanding of the specific goals to be achieved in the OR. | 625–629 | 0.66 (0.96) | 0.72 (0.94) | 0.55 (0.93) | <0.001 |
| Know clearly the task responsibilities of each team member. | 625–629 | 0.86 (1.07) | 1.01 (1.12) | 0.83 (1.15) | <0.001 |
| Achieve sufficient familiarity with how each team member will approach his/her task responsibilities (e.g. strengths, weaknesses, preferences) | 625–629 | 1.00 (1.10) | 1.20 (1.05) | 0.84 (1.04) | <0.001 |
| Have all of the anticipated human and material resources ready and ‘at hand’ for use. | 625–629 | 0.92 (1.08) | 1.07 (1.15) | 0.76 (1.09) | <0.001 |
| Use cues within the OR situation to coordinate my tasks with others. | 625–629 | 0.90 (1.03) | 0.94 (1.00) | 0.68 (0.95) | <0.001 |
| Use my understanding of a patient’s situation to anticipate team members’ needs. | 625–629 | 0.85 (1.11) | 0.82 (0.97) | 0.69 (0.91) | <0.001 |
| Monitor my own and other team members’ efforts to ensure that proper procedures and tasks occur as expected. | 625–629 | 0.87 (1.03) | 0.84 (0.90) | 0.67 (0.87) | <0.001 |
| Adapt my performance to accommodate changes that may occur. | 625–629 | 0.70 (1.07) | 0.70 (0.89) | 0.48 (0.90) | <0.001 |
| Use specific communication strategies to confirm that messages are received and the content is accurately understood (i.e. closed-loop communication). | 625–629 | 0.85 (1.03) | 0.92 (1.04) | 0.71 (1.01) | <0.001 |
| Interact with others to maximize their strengths and manage the workload effectively. | 625–629 | 0.84 (0.94) | 0.80 (0.98) | 0.60 (0.99) | <0.001 |
| Facilitate quality and continuous improvement (e.g. encouraging others, speaking up when concerns arise, offering critique). | 625–629 | 0.87 (1.06) | 0.83 (0.90) | 0.60 (0.93) | <0.001 |
| Use strategies effectively to promote team cohesion and effective work interactions. | 625–629 | 0.86 (0.96) | 0.81 (0.94) | 0.64 (0.88) | <0.001 |
| Use strategies to effectively provide feedback to OR team members. | 625–629 | 0.89 (1.02) | 0.86 (0.98) | 0.67 (0.88) | <0.001 |
| Use strategies effectively to resolve differences/disputes among team members. | 625–629 | 0.89 (1.10) | 0.81 (1.00) | 0.67 (0.87) | <0.001 |
| Average score | 625–629 | 0.84 (0.82) | 0.87 (0.79) | 0.66 (0.76) | <0.001 |
a Scale: definitely no = 1 to 6 = definitely yes.
b Mean (standard deviation).
c Paired two-tail t-test.
d All statistically significant after Bonferroni adjustment.

| T-TAQ subscalesa | Students (matched N) | Pre-training score, 2015b | Post-training score, 2016b | ∆: post–pre T-TAQa | p- valuec |
|---|---|---|---|---|---|
| Year 1 (2014–2015) | |||||
| All students | |||||
| Team structure | 80 | 4.62 (0.37) | 4.56 (0.42) | −0.07 (0.50) | 0.236 |
| Leadership | 80 | 4.73 (0.40) | 4.70 (0.39) | −0.03 (0.48) | 0.547 |
| Situation monitoring | 80 | 4.53 (0.44) | 4.55 (0.45) | 0.02 (0.44) | 0.718 |
| Mutual support | 80 | 3.19 (0.54) | 3.04 (0.43) | −0.16 (0.52) | 0.009 |
| Communication | 80 | 4.42 (0.43) | 4.43 (0.44) | 0.01 (0.43) | 0.813 |
| Trained students | |||||
| Team structure | 22 | 4.67 (0.34) | 4.60 (0.43) | −0.07 (0.48) | 0.493 |
| Leadership | 22 | 4.70 (0.37) | 4.68 (0.37) | −0.02 (0.49) | 0.886 |
| Situation monitoring | 22 | 4.58 (0.35) | 4.55 (0.43) | −0.03 (0.38) | 0.712 |
| Mutual support | 22 | 3.12 (0.33) | 2.94 (0.35) | −0.18 (0.51) | 0.108 |
| Communication | 22 | 4.36 (0.42) | 4.39 (0.42) | 0.03 (0.44) | 0.720 |
| Non-trained students | |||||
| Team structure | 58 | 4.60 (0.39) | 4.54 (0.42) | −0.06 (0.51) | 0.338 |
| Leadership | 58 | 4.75 (0.42) | 4.71 (0.40) | −0.04 (0.47) | 0.540 |
| Situation monitoring | 58 | 4.51 (0.47) | 4.55 (0.46) | 0.04 (0.47) | 0.556 |
| Mutual support | 58 | 3.22 (0.60) | 3.07 (0.45) | −0.15 (0.53) | 0.038 |
| Communication | 58 | 4.45 (0.43) | 4.45 (0.45) | 0.00 (0.49) | 0.960 |
| Year 2 (2015–2016) – All students | |||||
| Team structure | 43 | 4.63 (0.37) | 4.55 (0.37) | −0.08 (0.37) | 0.153 |
| Leadership | 43 | 4.76 (0.38) | 4.72 (0.35) | −0.04 (0.34) | 0.442 |
| Situation monitoring | 43 | 4.60 (0.45) | 4.51 (0.46) | −0.10 (0.44) | 0.160 |
| Mutual support | 43 | 3.32 (0.71) | 3.14 (0.49) | −0.18 (0.66) | 0.084 |
| Communication | 43 | 4.47 (0.39) | 4.43 (0.42) | −0.05 (0.40) | 0.394 |
| Year 3 (2016–2017) – All students | |||||
| Team structure | 51 | 4.50 (0.49) | 4.59 (0.48) | 0.09 (0.48) | 0.190 |
| Leadership | 51 | 4.55 (0.51) | 4.69 (0.42) | 0.14 (0.50) | 0.051 |
| Situation monitoring | 51 | 4.27 (0.53) | 4.46 (0.50) | 0.19 (0.60) | 0.027 |
| Mutual support | 51 | 3.11 (0.53) | 3.17 (0.51) | 0.05 (0.70) | 0.585 |
| Communication | 51 | 4.37 (0.48) | 4.42 (0.44) | 0.04 (0.48) | 0.527 |
a Scale: 1 = strongly disagree, 2 = disagree, 3 = neutral, 4 = agree, 5 = strongly agree.
b Mean (standard deviation).
c Paired two-tail t-test.
The interprofessional student team SBT was integrated into a pre-existing mandatory senior course that was part of the Curriculum of the School of Medicine. Known as Critical Concepts, this month-long course focused on emergency and critical care to prepare senior medical students for internship. It included an initial week-long period of simulation-based education in which students learned how to take care of urgent and emergent conditions in various specialties. The interprofessional student team SBT occurred mid-week in the morning of this period. All senior medical students, therefore, participated in the SBT, except for the first year of the program, which began in the middle of the academic year on January 2015. Second- and third-year nurse anaesthesia students enrolled in one of the nurse anaesthesia program’s practicum courses participated in these sessions. Finally, physical and occupational therapy students were drawn from various courses in their program.
Participants for the SBT sessions consisted of interprofessional teams of senior medical students, second- and third-year nurse anaesthesia students, physical therapy students, occupational therapy students and respiratory therapy students. Team composition evolved over the course of implementation. From January 2015 to June 2015, they consisted of senior medical students and nurse anaesthesia students. For the following academic year, July 2015 to June 2016, teams transitioned to senior medical students, nurse anaesthesia students and occupational therapy students. In the final academic year of implementation, July 2016 to June 2017, physical therapy students and respiratory therapy students began participating on the medical and nurse anaesthesia student teams.
In general, interprofessional student teams were composed of six members, two members from each of the three professions participating in the SBT session. At least one member from each specialty participated in each training session. Within each profession, one member assumed a senior role with the other playing a junior role for the first scenario, switching the roles for the second scenario. In situations where fewer or more team members participated in a SBT session, the scenarios eliminated the junior role or added other mid-level roles, respectively.
Training scenarios focused on a patient with a behavioural health disorder who underwent rapid clinical deterioration due to an underlying illness. Thus, scenarios created a clinical situation leading to the need for a rapid response or code resuscitation of the patient. This situation led to rich discussion about teamwork in the after-action debriefing.
Evaluation of the interprofessional student team SBT followed Kirkpatrick’s framework to assess the effectiveness of training programs [25]. For Level 1 data, at least two investigators developed themes related to responses independently and then reached agreement together for verification.
For Level 2 data, mean TAS subscale scores for observers and participants ratings were determined for all first-time participants with one-way ANOVA evaluating the difference between mean calculated observer- and participant-rated performances after each scenario for each year of the program. The TAS tool has evidence of both convergent validity [20] and generalizability [18]. For the Readiness for Interprofessional Learning Scale (RIPLS) questionnaire [26], mean item scores were determined, and paired samples t -test with Bonferroni correction was calculated for each matched pre-/post-session item score for each year of the program. The RIPLS questionnaire is widely used in the literature [27], having undergone subscale modification [28]. Finally, mean scores for each item were determined for the Interprofessional Teamwork (IPT) questionnaire [19,21] and paired samples t-test with Bonferroni correction calculated for each matched pre-/post-session item score.
For Level 3 data, mean TeamSTEPPS™ Teamwork Attitudes Questionnaire (T-TAQ) subscale scores were determined for each year of the program, and one-way ANOVA calculated to determine the difference between mean calculated medical student score at the beginning of academic year in June and upon graduation in April of the same academic year for each year of the program. The T-TAQ has undergone scale reliability and correlation testing [29,30]. For the 2015 academic year, T-TAQ scores were further divided between those students who did not undergo interprofessional student team SBT and those who did. Senior medical students who had participated in the Critical Concepts course from July to December of 2014 did not have the opportunity to participate in the SBT. Those who had taken the Critical Concepts course from January to June of 2015 had undergone SBT. Note, SBT training only went from January to March, since senior students participated in a class-based course in April and graduated in May. Differences between 2015 subscale scores of non-trained and trained students were calculated using paired samples t-test with Bonferroni correction. Finally, trends in subscale scores from year to year of each medical school class were analysed using linear regression.
For each survey, students used a personal identification number that they self-generated in order to match pre-/post-intervention evaluations as well as to compare with other evaluations that the student completed. For each statistical analysis, any incomplete paired data set was discarded prior to comparison using an ad hoc method.
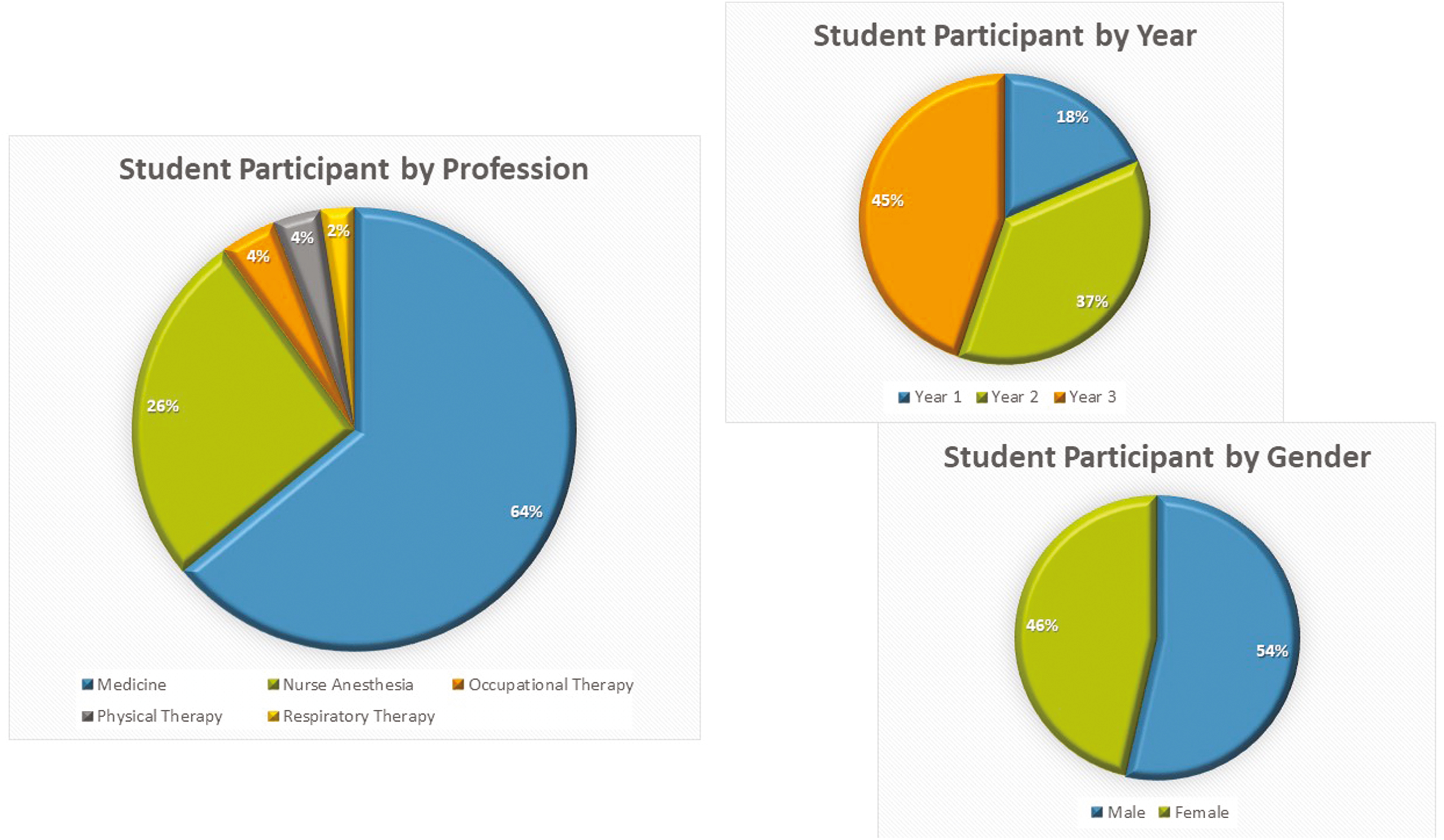
Figure 1 details participant breakdown over the course of the program. In brief, a total of 727 participants attended sessions, of which 659 were first-time attendees and 68 were repeat attendees, all of whom were nurse anaesthesia students. Overall, among first-time attendees, 422 were medical students, 171 were nurse anaesthesia students, 27 were occupational therapy students, 23 were physical therapy students and 16 were respiratory therapy students. Gender distribution of first-time attendees was 353 males and 306 females.

Overall, participant reaction to the SBT was favourable. Participants responded in the affirmative when verbally asked after completion of the second debriefing whether the interprofessional student team training was worthwhile. In general, responses fell into the following main themes: (1) interprofessional learning, (2) team collaboration, (3) authenticity of experience. Students expressed appreciation for the opportunity to engage in an IPE activity. They stated that they learned about the experiences, background, responsibilities and strengths of students from other professions during the SBT. This learning led to insights that they believed would help them work with other professions in the clinical setting.
Participants also expressed that they enjoyed practicing team collaboration with other professions. They believed that such team SBT was superior to the usual SBT they participated in when only their profession was present. Such interprofessional SBT would help them be more effective in clinical practice related to their contribution to team activities.
Finally, participants liked the authenticity of the SBT scenarios. During debriefing reflection, participants stated that the clinical setting was more accurate given the interprofessional character of the teams and the format of the scenarios. In fact, they often requested that more such SBT sessions with interprofessional students be scheduled, replacing the other SBT format. This sentiment was typically expressed when they were asked how the sessions could be improved.
Figure 2a–c summarizes the significant self-, peer- and observer-rated mean score changes from the first to second SBT scenario for interprofessional student team performance in the three TAS subscales for each year of the program. In brief, data were available for between 238 and 244 interprofessional student team SBT encounters. Ranges for the total number of evaluations for TAS subscales for self-, peer- and observer-based ratings were as follows: (1) TBB – self-rated range 592–607, peer-rated range 717–718, observer-rated range 690–694; (2) SMM – self-rated range 478–488, peer-rated range 478–488, observer-rated range 238–243; and (3) ACR – self-rated range 468–487, peer-rated range 468–487, observer-rated range 241–244. Overall, statistically significant mean increases on each subscale score occurred for every year of SBT of interprofessional student teams. For self-rated TAS subscale scores, mean increases from scenario 1 to scenario 2 ranged from 0.45 to 0.6 units for TBB, 0.71 to 1.59 units for SMM and 0.76 to 1.64 units for ACR. For peer-rated TAS subscale scores, mean increases from scenario 1 to scenario 2 ranged from 0.28 to 0.58 units for TBB, 0.71 to 1.59 units for SMM and 0.76 to 1.64 units for ACR. For observer-rated TAS subscale scores, mean increases from scenario 1 to scenario 2 ranged from 1.21 to 1.42 units for TBB, 1.57 to 1.62 units for SMM and 1.39 to 1.54 units for ACR.

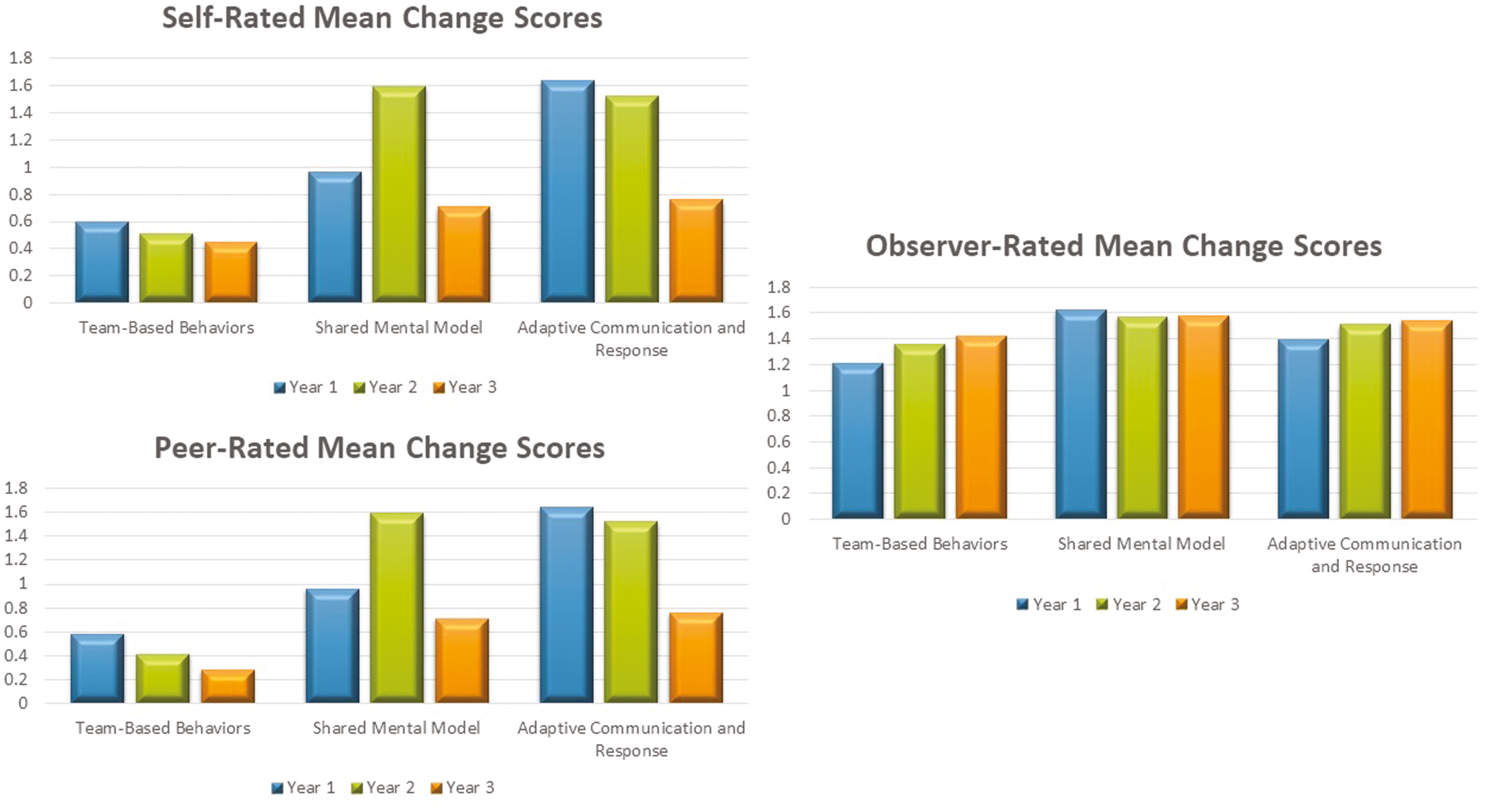
Figure 3 summarizes the findings from analysis of the RIPLS and IPT mean item score changes from pre- to post-session for every year of the program. In brief, the range of completed, matched RIPLS evaluations was from 646 to 649. Statistically significant increases (decreases for negatively worded items) were present for 11 items across all 3 years, including the overall mean change combining all 19 items. Of these 11 items, six items demonstrated a mean item score change of 0.20 units or greater across all 3 years. They included items related to shared learning: clarifying the nature of patient problems, helping one become a better team worker, aiding one in thinking positively about other professions and increasing one’s ability to understand patient problems. In addition, they included items related to improving relationships with other professions after qualification and a willingness to work with other healthcare students on small group projects. The 11 individual mean item score improvements that occurred each of the 3 years of the program clustered in questions related to the teamwork and collaboration subscale as well as the positive professional identity component.

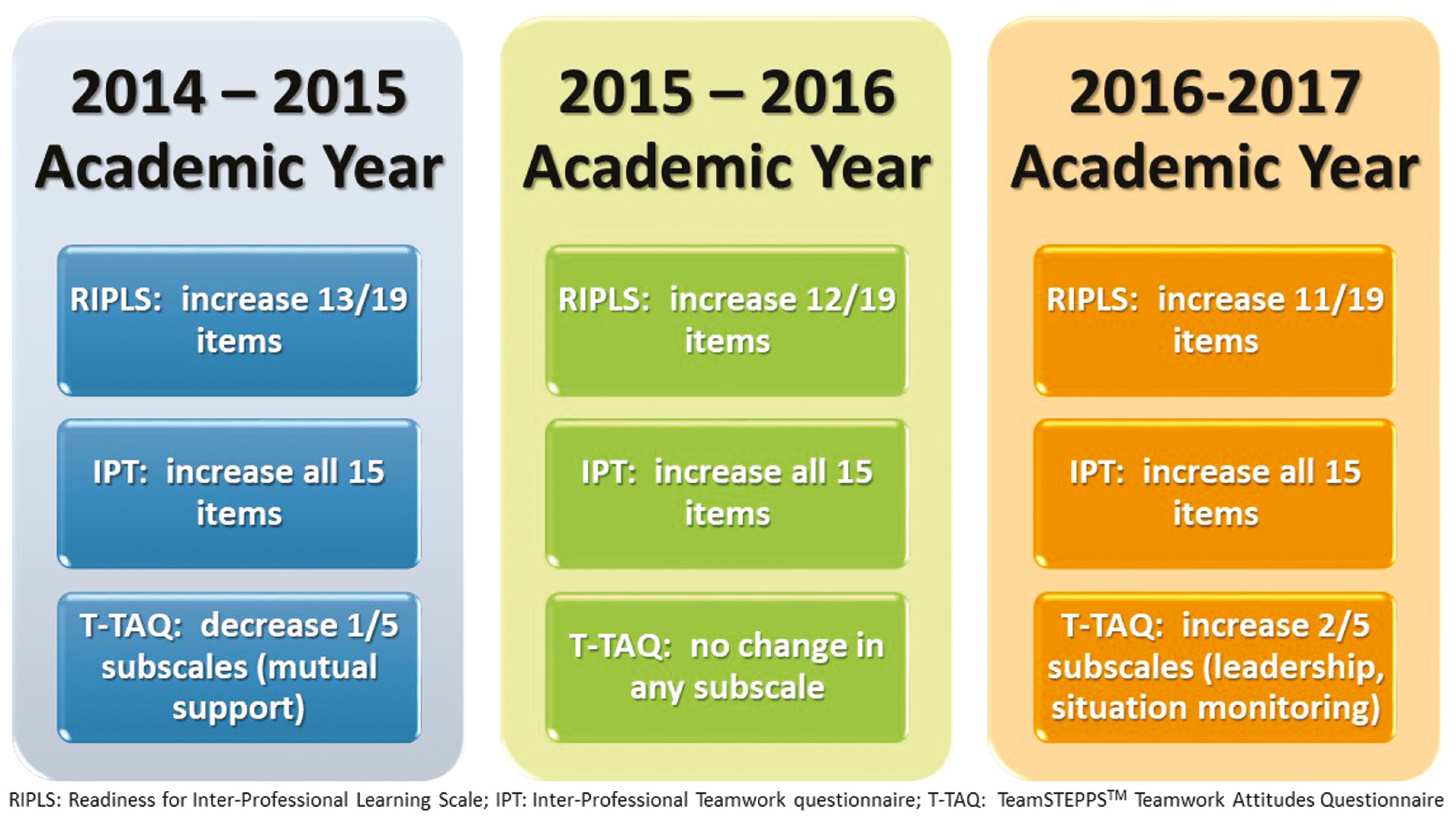
Statistically significant RIPLS mean-item increases (decreases for negatively worded items) for only 1 year of the program were present for three items (Year 1 for two items and Year 2 for one item). No statistically significant change in mean item scores occurred for five items. Of the five individual mean items that failed to show any significant change in any of the 3 years of the program, one item was in the teamwork and collaboration subscale, two were in the negative professional identity component and two were in the roles and responsibilities subscale.
The range of completed, matched IPT evaluations was from 625 to 629. Statistically significant increases were present for every item for every year of the interprofessional student team SBT. These increases ranged from 0.5 to 1.20 units, representing improvements of 8.3% to 20% of the 6-point scale score. The relative improvements were even higher, given scores on the lower end of the scale (i.e. 1 and 2) were rare to non-existent.
Changes in the IPT mean item scores ranged from 0.63 to 1.00 units for Year 1, from 0.70 to 1.20 units for Year 2 and from 0.50 to 0.84 units for Year 3. Overall, average mean change scores for all 15 items for each year had statistically significant improvements. These increases ranged from a low of 0.66 for Year 3 to a high of 0.87 for Year 2.
Figure 3 also summarizes the analytical findings for overall T-TAQ mean subscale scores for matched medical students for each year of the program. In brief, 174 students completed pre- and post-intervention T-TAQs over the 3-year period, 80 for Year 1, 43 for Year 2 and 51 for Year 3. In Year 1, 58 students who completed matched T-TAQs did not undergo SBT, and 22 students did participate in the SBT. A statistically significant decrease in the mutual support subscale overall occurred in Year 1 (mean scores 3.19 ± 0.54 2014 to 3.04 ± 0.43 2015, Δ = −0.16 ± 0.52, p = 0.009). It also occurred for non-trained students in Year 1 (mean scores 3.12 ± 0.60 2015 to 3.07 ± 0.45 2016, Δ = −0.15 ± 0.53, p = 0.38). A statistically significant increase in situation monitoring occurred in Year 3 (4.27 ± 0.53 2016 to 4.46 ± 0.50 2017, Δ = 0.16 ± 0.60, p = 0.027). No statistically significant change in mean T-TAQ subscale scores occurred in Year 2 or for the remaining subscale scores for Years 1 and 3. In Year 3, the mean subscale positive change in leadership was near significant (4.55 ± 0.51 2016 to 4.69 ± 0.42 2017, Δ = 0.14 ± 0.50, p = 0.51).
Trend analysis of mean subscale T-TAQ score changes revealed statistically significant positive increasing trends from Year 2 to Year 3 in leadership ([Year 2 − Year 3] = −0.18, mean 0.44, p = 0.04) and situation monitoring subscales ([Year 2 − Year 3] = −0.29, mean 0.53, p = 0.009). Further analysis of these two positive results across all 3 years revealed a statistically significant increase in leadership scores from 2015 to 2017 (p = 0.049). No significant increase was present in situation monitoring scores from 2015 to 2017 (p = 0.09).
Our findings indicate that one 2-hour, high-fidelity SBT session of a combination of interprofessional students from medicine, nurse anaesthesia, physical therapy, occupational therapy and respiratory therapy demonstrated Kirkpatrick [39] Level 1 and 2 training effectiveness. Student reactions to the SBT session were very positive and emphasized the benefit of interacting in an educational setting with students from other professions. Such reactions led to an attitudinal change in students’ perceptions of IPE in general, as demonstrated by an increase (decrease for negatively worded items) in mean item scores for 11 out of the 19 RIPLS items across all 3 years of the program.
Clearly, health professional students appreciate IPE, an observation supported in this study and in the literature. For example, Costello et al’s [31] qualitative examination of student experiences of interprofessional simulation delineated three themes related to such SBT: (1) increased understanding of the role of professionals, (2) increased sense of confidence and ability to improve patient outcomes and (3) increased appreciation for interprofessional simulation as a valuable learning experience. Additionally, Paige et al [34], as part of the authors’ work, found a similar theme of valuing interprofessional collaboration among participants’ responses to verbal inquiry about the SBT experience in the team training for emergency room trauma transfers (TTERTT) program involving undergraduate nursing students training with surgical and emergency medical residents. Furthermore, as noted by students undergoing SBT in the current study, Reime et al [32] found that medical students valued the enhanced realism that interprofessional student team SBT provided. In addition, Reime et al [33] found that students preferred learning by doing through participation in an SBT activity versus observation. Escher et al [33] demonstrated that medical students’ intrinsic motivation to participate in team SBT increased after undergoing such a training. These observations reveal that health professional students, like the ones in the current study, understand and value the benefits of IPE.
Participation in SBT of interprofessional student teams also helps students to develop positive perceptions of other professions. Such findings are consistent with other studies involving health professional students in the literature. For example, Wellmon et al [34] found that high-fidelity SBT of code resuscitation involving an interprofessional team of physical therapy and nursing students improved RIPLS scores related to teamwork and collaboration as well as professional identity. This team training also led to improvement in the competency and autonomy as well as the perceived need for and perceptions of actual cooperation subscales on the Interdisciplinary Education Perception Scale (IEPS); it also led to high scores related to team value and efficiency on the Attitudes Toward Health Care Teams Scale (ATHCTS). Burford et al [35] showed improvements in the RIPLS(Core) score for interprofessional teams of medical and nursing students participating in three acute care SBT scenarios. Nursing students tended to have higher RIPLS(Core) scores than medical students. Such training also seemed to enhance professional identity as related to emotional aspects of group membership, especially with nursing students. Finally, as part of the authors’ work, Leithead et al [36] found improvements in RIPLS overall scores for medical and nurse anaesthesia students, but not undergraduate nursing students, participating in interprofessional student operating OR training using high-fidelity SBT. The benefit of conducting IPE earlier in a clinician’s career, when students are more receptive to attitudinal change, rather than later, when interprofessional attitudes are more rigid due to the cultural environment, becomes apparent with such findings. The authors’ own work related to the TTERTT program, in which only 2 of the 19 items of the RIPLS questionnaire demonstrated statistically significant improvements, reinforces this view.
Equally important as the attitudinal improvement related to IPE, the 2-hour high-fidelity SBT sessions resulted in the participating health professional students learning knowledge, skills and attitudes (KSAs) related to teamwork and team processes. Thus, students’ self-efficacy towards team-based competencies improved with the training. Again, this finding supports other research in the literature related to teamwork training and self-efficacy. For example, Tofil et al [37] demonstrated that SBT of interprofessional teams of medical and nursing students focusing on internal medicine topics improved communication self-efficacy of both professions. Paull et al [38] demonstrated increases in self-efficacies related to teamwork and communication after in situ SBT interprofessional team training of post-operative staff within the Veterans Administration hospital system. Egenberg et al [39] found that improvements in self-efficacy and collective efficacy after SBT of interprofessional teams related to post-partum haemorrhage and that such training led to clinical outcome improvements related to transfusion requirements. The authors’ prior research has confirmed SBT’s positive impact on self-efficacy towards team-based competencies when training interprofessional student teams [18–21]. Given the link between self-efficacy and behavioural change [40,41], the positive changes in the current study suggests that the SBT primes students for modelling such behaviours in the clinical setting. Even if such a link is controversial, the SBT serves as a strong motivator for improving team behaviour among participants.
Most notably, the 2-hour high-fidelity SBT of interprofessional student teams led to participants learning team-based competencies that they were able to put into action. Throughout all 3 years of the program, interprofessional teams improved their observer-rated team performance from the first scenario to the second scenario based on the TAS instrument. This improvement was for individual team-based behaviours as reflected in the TBB subscale as well as for overall teamwork and interaction as measured by the SMM and ACR subscales. Again, such improvement in team performance occurs in the literature. For example, Jakobsen et al [42] documented that trauma team SBT of nurse anaesthesia, medical and nursing students led to enhanced observer-rated performance of students’ leadership and communication skills. Nurse anaesthesia students scored higher than either medical students or nursing students, and they struggled less with finding their role. Nelson et al’s [12] review of interprofessional team training of pre-licensure students resulted in improvements in team knowledge, communication and skills. These findings align with the authors’ own work training a wide variety of health professional students [18–21]. Such findings explain the popularity of SBT for developing teams in healthcare. Given the fact that interprofessional team SBT has also improved work place culture in high acuity settings [43,44], the consistent learning of team-based competencies over the 3 years of the SBT suggests that such a team development intervention could help students recognize and avoid pernicious aspects of the hidden curriculum such as the modelling of ineffective behaviour patterns.
The training format and scenario design definitely contributed to the learning effectiveness of this particular interprofessional team SBT. In particular, the dual-scenario structure with immediate after-action facilitator-guided structured debriefing was an especially effective design. It enabled participants to reflect on their SBT experience and team performance in a timely manner. Furthermore, it allowed them to identify team performance gaps, learn about team-based competencies that may address them, and, most importantly, gave students the opportunity to practice applying the team-based competencies to the performance gaps in a deliberate manner during the second scenario of the session. In this way, they could embed learning through such deliberate practice of behaviours. Additionally, each session began with a brief that reviewed learning objectives, ground rules and the scenario background. These features of incorporating debriefing into the SBT, allowing for deliberate practice of skills and providing a brief as well as debrief are recognized best practices of simulation-based education in healthcare [45]. Furthermore, Eddy et al [46] found in their systematic review of health professionals’ experience of teamwork education in acute care settings that participants valued teamwork education that created authentic learning opportunities and fostered reflection and debriefing. Such opportunities increased participants’ confidence and motivation to apply the teamwork skills they learned. Coppens et al [47] showed that incorporating a debriefing following an SBT scenario to teach crew resource management techniques was more effective at increasing participants’ self-efficacy and team efficacy than SBT without debriefing. Finally, dividing team members at the beginning of the scenario such that only two members were in the patient room to begin the SBT reflected what would be encountered in the clinical setting, adding to the authenticity of the learning opportunity so valued by participants [47].
Since the TAS can serve as a multi-source evaluation (MSE), participants were able to rate themselves and their peers after each SBT scenario. As with the observer-rated TAS scores, the self- and peer-rated TAS subscale mean change scores all increased from the first to second scenario across all 3 years of the program. For the TBB, mean score changes were lower than the observer-rated changes, consistent with prior findings from the authors’ work in which participants tended to over-estimate their own and peer scores [18,20,21]. Such inflation of performance scores is well known in the professional degree [48] and healthcare literature [49–51].
Although this interprofessional team SBT program demonstrated effectiveness related to participant reactions and learning, its effectiveness related to instilling behavioural change was less convincing and more nuanced. For example, the T-TAQ completed by medical students at the beginning and end of their academic year only demonstrated a statistically significant negative change in mutual support in Year 1 (Δ = −0.16, p = 009). This cohort, however, included medical students who had completed the Critical Concepts course the first half of the academic year, and, therefore, had not undergone the interprofessional team SBT. When these non-trained students were separated from those who had trained, the only statistically significant change among the two groups was a negative one in mutual support in the non-trained cohort of medical students (Δ = −0.15, p = 0.038). Such a finding suggests that the overall Year 1 negative finding is likely due to the incorporation of the non-trained medical student mean subscale scores into the overall Year 1 analysis. Interestingly, comparison of the T-TAQ subscale scores between the trained and non-trained students did not reach statistically significance. Year 2 did not demonstrate any statistically significant changes in the T-TAQ subscales, but Year 3 did have a statistically significant positive change in situation monitoring (Δ = 0.19, p = 0.027) as well as a positive trend in leadership (Δ = 0.14, p = 0.051). Linear trend analysis demonstrated statistically significant improving trends from Year 2 to Year 3 for situation monitoring and leadership, and a Year 1 through Year 3 statistically significant improvement in leadership. In the authors’ earlier work, Paige et al [20] found statistically significant improvements in team structure and mutual support overall for medical students completing the T-TAQ at the beginning and end of their academic year. When divided into trained and non-trained medical students, a statistically significant difference existed in team structure scores, suggesting the training had a positive impact on this subscale.
A strength of this study is its scope. It is one of the few investigations to follow a SBT team development intervention over a multi-year period. As a result, close to 700 student encounters with the SBT intervention occurred, involving five separate student healthcare professions. This 3-year prospective investigation of an SBT program with demonstrated learning effectiveness throughout the entire period is an example of a successful integration of a SBT curriculum into a health sciences centre. Key to this success was incorporating it into an established course structure within the School of Medicine. Integrating the SBT sessions into the Critical Concepts course ensured that all medical students would undergo training. Additionally, it provided a time and space for conducting the SBT. In this manner, the SBT was not a stand-alone endeavour, but it was instead part of the course structure. Such integration into existing curricula is a recognized strategy to ensure implementation success [13,52]. Finally, successful implementation was also due to adherence to accepted principles of team training, such as identifying critical teamwork competencies to use in training, emphasizing teamwork over task work, employing simulation-based scenarios that reflected the clinical environment, providing outcome-based and behaviour-based feedback and determining program effectiveness [46].
Limitations to this study do exist. Although the study included over 700 student encounters and health profession students from five different specialties, all participants were students at the LSU Health New Orleans Health Sciences Center, and the simulations took place in the same location. This fact limits the generalizability of our findings of this large undertaking in SBT. Additionally, despite pleas to student participants to avoid discussing the simulations with fellow students who had not yet participated in the SBT sessions, it was not possible to ensure that first-time participants were naïve to the scenarios they experienced. As a result, students might have performed better than expected from anticipating the medical emergencies that they would encounter during the SBT session. Finally, the ability of the mannequin to respond to participants’ initial screening questions at the start of the scenarios was somewhat limited to pre-recorded responses. This fact may have hampered the students in asking the key behavioural screening questions related to mental health disorders.
Another limitation related to the collection method for the annual T-TAQ administered at the beginning and end of each academic year. At the beginning of each academic year, the authors were able to distribute the T-TAQ for voluntary completion at a mandatory administrative gathering of the incoming fourth-year medical students. This situation optimized the number of potential respondents. Administration of the end of the year T-TAQ, however, occurred during a purportedly mandatory Special Topics session held just before fourth-year student graduation during the final month of the students’ medical school training. One of the authors distributed it just before giving one of the lectures during this series. Student participation in completing the T-TAQ was lower in this situation due to poor attendance at the lecture and general lack of enthusiasm for completing any further surveys or forms just before graduation. The low number of matched T-TAQ forms (only 174 matched results, of which 58 represented non-trained students), therefore, represented only a fraction of the actual fourth-year medical student class that had participated in SBT sessions, limiting our findings related to changes in attitudes over the academic year. Clearly, trying to tease out a link between a 2-hour training session in interprofessional student SBT and behavioural change over the course of an academic year is difficult and fraught with the possibility of confounding variables influencing results.
In conclusion, students seem to value interprofessional collaboration fostered by participation in a high-fidelity, simulation-based, interprofessional team training program across a health science centre. Such a SBT program has a positive immediate impact related to attitudes towards readiness for interprofessional learning as well as team-based attitudes and learning of team-based behaviours. Longer-term attitudinal changes related to teamwork are more difficult to determine with sporadic improvements in attitudes towards selected team-based competencies. Given its effectiveness in allowing participants to learn team-based competencies, an interprofessional student SBT curriculum using high-fidelity, simulation-based techniques has the potential to breakdown the silo mentality of clinical practice early in healthcare professional student training.
None declared.
This project is a 3-year intervention funded by the United States Health Resources and Services Administration (HRSA). It was part of a HRSA 14-066 Advanced Nursing Education (ANE) Program Grant Award (No. D09HP26947).
Data available on reasonable request and with adherence to confidentiality.
None declared.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.