
Interprofessional simulation-based learning provides collegiate students with safe, realistic scenarios to learn and refine vital health related skills. This article describes an innovative project that engages college students from various disciplines in simulation-based activities to enhance health and professional knowledge, promote safety awareness, and improve cultural sensitivity. Additionally, the theme of traveling domestically and/or abroad during spring break provided a true-to-life backdrop.
The Activity Theory provides the framework for this study emphasizing collaborative learning toward shared goals. Six spring break themed simulation scenarios were created and evaluated using a mix-methods design. Pre-posttest measures were conducted using the Student Perceptions of Interprofessional Clinical Education-Revised Instrument, and open-ended responses.
Twenty-eight students completed the survey showing statistically significant change scores from pre-post. Qualitative findings identified three overarching themes of participants’ gains: 1) knowledge of other healthcare professionals’ roles, 2) healthcare professions’ contributions to patient care, 3) being respectful of other cultures, being prepared when traveling, and knowing how to improvise while traveling abroad.
Students enjoyed a meaningful and engaging interprofessional activity while learning about one another’s professions, appreciating other healthcare professions’ roles, developing awareness and respect for other cultures, and practicing skills that may be needed during challenging encounters while traveling.
What this study adds
Spring break is a rite of passage for many college students. It is welcomed as a time for rest, fun, exploration and socialization. Many students will travel abroad during spring break, which can contribute towards additional barriers to staying safe. In addition, it is also a time that some will engage in risky or careless behaviours that can result in adverse events [1,2]. Injuries from alcohol and other substance use, driving while under the influence and taking risks with personal safety all increase during spring break [1,3,4]. When events become harmful or dangerous, college students may lack the experience and knowledge to manage the situation, especially in unfamiliar locations. Additionally, developing cultural awareness and respect are essential skills for travelling abroad on spring break.
Simulation is an engaging teaching methodology designed to immerse students in realistic healthcare scenarios that enable them to learn in a safe space [5]. Substantial research shows this evidence-based learning pedagogy is effective for skill training and confidence building [6,7]. Interprofessional simulation, where students from two or more professions engage with one another, lends itself to active learning experiences as it promotes student collaboration and interaction with other disciplines [8,9], fosters interprofessional communication and enhances students’ learning from and with one another [10]. Many healthcare programs, including nursing, athletic training, medicine, pharmacy, dentistry and social work, either mandate or strongly encourage student involvement in interprofessional education during their healthcare curricula [11].
This article describes a novel project designed to immerse college students in an interprofessional simulation-based activity to enhance knowledge of one another’s professions, promote awareness of safety, improve knowledge related to managing adverse/preventable situations and enhance the development of cultural competence and a global perspective for students travelling domestically and/or abroad during spring break. In addition, we describe the development and implementation of a spring break-themed interprofessional simulation activity and the simulation assessment from the healthcare students’ perspectives.
Evidence shows engaging students in the learning process facilitates increased knowledge, increased confidence and improved attitudes towards teamwork [10,12]. Further studies highlight that making learning fun has been correlated with improved student success [13–15]. This project used Activity Theory as the theoretical framework. Activity Theory posits that learning occurs and is co-constructed as students collaborate with one another to achieve shared goals [16]. This framework is highly applicable to interprofessional simulation-based learning [16,17] as students learn by engaging with one another to optimize client care and learn about one another’s professions. The attributes of the project as they correspond to Activity Theory are demonstrated in Figure 1 [18].

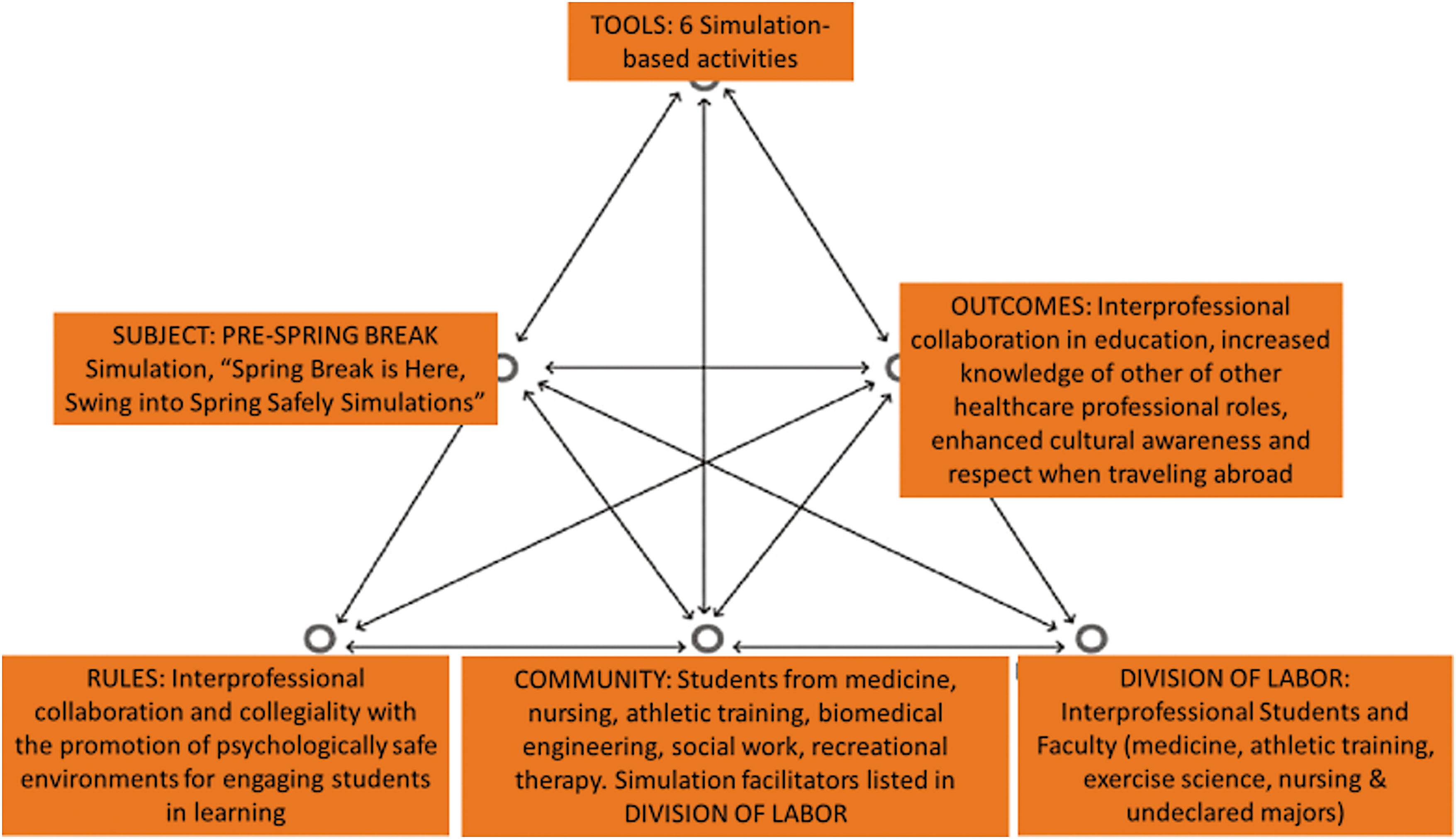
Activity Theory framework for interprofessional simulation activity
This study included an interprofessional simulation educational activity for diverse groups of healthcare students at an academic university in the southeastern United States. A pre-posttest survey design was used for assessment. The authors’ University Institutional Ethical Review Board approved this educational activity as an exempt study (H23-0618). We used the CONSORT simulation guidelines developed by Cheng et al. to highlight what was planned, done, found, and concluded [19].
In this activity, a diverse group of interprofessional healthcare college students participated in six spring break-themed simulation scenarios. The spring break theme provided opportunities to immerse students in scenarios designed to promote safety awareness and foster cultural sensitivity awareness in a simulated interprofessional educational activity. The team designed and implemented the event and named it the ‘Spring Break is Here, Swing into Spring Safely Simulations’.
An interprofessional team of faculty and staff from the college designed the simulation activity. In accordance with the Health Care Simulation Standards of Best Practice, learning outcomes were identified, and scenario objectives were developed [20]. Table 1 highlights the simulations’ objectives, designs and student activities. The planning team consulted content expert faculty from across the college and community partners such as a Regional Trauma Coordinator to ensure the simulated scenarios were realistic and evidence-informed. The team met weekly for 3 months to design the activity. Six interprofessional simulation scenarios were designed to be engaging for a diverse group of healthcare students. The content of the simulations was on an introductory level with the goal of being inclusive of all healthcare students regardless of their individual education level.

| Scenario: Health event | Objectives: Upon completion of this activity, students will collaborate on interprofessional teams to: | Scenario/vignette | Student interprofessional collaboration activities: |
|---|---|---|---|
| Fun in the Sun: Heat Stroke | • Define heatstroke. • Identify abnormal findings related to heatstroke and sunburn. • Demonstrate initial care protocol for heatstroke. • Discuss their professions’ role in heatstroke prevention, management and rehabilitation. |
Two hikers in Mexico without adequate water, food and directions, lost in the Mexican desert, develop symptoms of heatstroke. | Worked in teams to identify symptoms of heatstroke, developed and executed a treatment plan to get the hikers to safety. |
| Shark Bite: Stop the Bleed Initiative | • Demonstrate how to effectively apply pressure to a wound. • Implement the correct method of packing a wound to control bleeding. • Demonstrate the correct application of a tourniquet. • Discuss alternatives for a tourniquet when none is available. • Discuss their professions’ role in managing trauma. |
Students are relaxing on a beach in South Africa when a shark bites a surfer. | Worked in teams using ‘Stop the Bleed’ skills to treat a shark bite victim. |
| Pour It Up: Alcohol Awareness | • Define binge drinking. • Describe increased health risks associated with excessive alcohol consumption. • Identify abnormal findings related to binge drinking. • Demonstrate initial care protocol for binge drinking. • Discuss their professions’ role in alcohol use/misuse, prevention, management and rehabilitation. |
Students attend a party on a Caribbean cruise ship. | Played a simulated drinking game and collaborated in an online gameshow designed to increase awareness of alcohol volume, concentration, binge drinking, symptoms of and management for, an alcohol overdose. |
| Pardon My French: Cultural awareness and respect for travel abroad | • Identify strategies to develop cultural awareness/respect/humility. • Identify potential safety hazards related to travelling abroad. • Discuss strategies to minimize risk related to travelling abroad. |
Students are sitting in a Paris café. The students are unable to speak French to order food. | Collaborated to devise strategies to be better prepared to respectfully engage when travelling abroad. |
| Heart on the Court: CPR and AED skills and awareness | • Identify signs and symptoms of a Sudden Cardiac Arrest. • Demonstrate high-quality chest compressions. • Demonstrate the application of an AED. • Discuss their professions’ role in cardiac emergency management. |
Fans are cheering at a basketball game, and suddenly one fan suffers a cardiac event | Students collaborated to identify pulselessness, begin high-quality CPR and apply an AED. |
| ‘Yes, I can Say No’: empowering students to say ‘no’ when they find themselves in uncomfortable and/or unsafe circumstances | • Identify how one can say ‘no’ in uncomfortable situations. • Discuss their professions’ role in empowering students/patients to say ‘No’. |
Students sitting on picnic blankets around a campfire enjoying friendship and conversation. | Students practiced communication skills by saying ‘No’ to one another in a series of increasingly complex scenarios. |
Prior to the event, the simulation educators offered a dress rehearsal session for faculty facilitators to practice their scenarios and learn about debriefing methods. Faculty facilitators were identified as interprofessional champions at the university. Facilitators were trained in both simulation facilitation and debriefing methods following the Health Care Simulation Standards of Best Practice [21,22].
The simulations were designed to expose students to basic safety events that require emergency management skills relevant to all healthcare professions. The rationale for this focus was that if students found themselves in emergency situations, skills such as beginning cardiopulmonary resuscitation, applying an automated external defibrillator (AED), treating symptoms of heatstroke, managing a hemorrhage and recognizing alcohol-related illnesses are pertinent, timely and essential skills all healthcare students should be able to perform. Additionally, four of the simulation scenarios were designed to engage students in scenarios encouraging cultural awareness and sensitivity. Finally, the interprofessional nature of these scenarios immersed students in a meaningful activity intended to enhance their knowledge of other healthcare professions’ roles, responsibilities and skills through collaboration and discussion.
The Spring Break is Here: Swing into Spring Safely interprofessional simulations were implemented during a 2-hour evening event. The simulations were conducted in six multi-use problem-based learning rooms designed for student collaboration. Volunteer students and faculty decorated the rooms and hallway with beach-themed and travel abroad décor. Each 15-minute scenario was conducted six times to allow 55 students to participate in groups of 8–10, and the remaining time was used for Prebriefing, survey completion and an informal reception that served as a forum to encourage further information sharing, collegiality and networking. Groups were intentionally mixed to consist of interprofessional students from different disciplines.
Each simulation scenario began with students and facilitators introducing themselves and identifying their profession. Next, volunteer simulated participant actors conducted a 1- to 2-minute skit/vignette that set the stage for the scenario’s objectives. Simulated participant actors were trained for role portrayal prior to the activity following the Association of Standardized Patient Educator Standards of Best Practice [23]. Table 1 outlines each scenario vignette.
Acknowledging that some of the students who participated in the simulations were from other universities, involving their faculty in the simulation was necessary to further build collaboration and community. Faculty from other universities were invited to attend virtually using an online video platform attached to a telepresence robot. The robot is essentially a tablet device on a segway that allows the virtual guests to travel from room to room with the in-person students.
At the end of each simulation, facilitators guided a debrief session to review the scenario content, emphasize key points and engage the students in discussions that highlighted how their respective profession would engage in and manage the scenario/vignette topic, and describe the typical places/environments the event might occur in their practice(s) how and where their respective professions might be involved in the treatment of such an event.
At the end of the simulation activity, participants were asked to complete the Student Perceptions of Interprofessional Clinical Education-Revised Instrument, version 2 (SPICE-R2) survey and answer open-ended response questions via Qualtrics. The SPICE-R2 is a psychometrically validated 10-question survey that assesses students’ attitudes towards interprofessional healthcare teams and the collaborative approach to client/patient care using a 5-point Likert-like scale (1 = strongly disagree to 5 = strongly agree) (Cronbach alpha = 0.86) [10,24,25]. The survey was administered before and immediately following the simulations. Additional open-ended questions developed by the team were used to obtain more detailed reflection and feedback on students’ perspectives of the simulations and their perspectives on the value of the interprofessional experience. The academic and clinical performance of the students during the simulation was not formally evaluated as this was a formative simulation experience.
Descriptive characteristics of the students were summarized using appropriate univariate statistics: Mean ± SD or N (%). Within-student change in SPICE-R2 scores was analysed using Student’s paired t-test. Statistical significance was determined at p < 0.05. All analyses were conducted using SAS v9.4 (SAS Institute, Cary, NC).
Content analysis was used to develop thematic findings. As a first step to content analysis, all open-ended response data were read line by line multiple times by the analysis team (JV, TA, SS, LHS). The analysis team began with no pre-existing assumptions or theories about the data [26,27] and proceeded with a systematic approach to reviewing and interpreting the data to illustrate student perspectives. Data were analysed using verbatim text, separated into initial codes and documented using an audit trail. Codes were sorted into categories and carefully interpreted into overarching themes [26,27]. Four peer debriefing sessions were conducted with the analysis team to enhance the validity of the qualitative findings.
Fifty-five total students participated in the interprofessional simulations and Table 2 shows the breakdown by discipline.

| Discipline | Number |
|---|---|
| Medicine | 20 |
| Athletic Training | 19 |
| Exercise Science | 1 |
| Nursing | 11 |
| Not enrolled in their major/undeclared | 3 |
| Other | 1 |
The 15 facilitators represented seven interprofessional areas of expertise (Table 3).

| Discipline | Number |
|---|---|
| Athletic Training | 2 |
| Biomedical Engineering | 1 |
| Nursing | 5 |
| Social Work | 4 |
| Recreational Therapy | 1 |
| Medicine | 1 |
| Trauma Expert | 1 |
Twenty-eight students completed pre- and post-simulation SPICE-R2 scores (51% survey response rate). The mean SPICE-R2 scores at pre- and post-simulation were 41.0 ± 3.9 and 44.4 ± 4.5, respectively. The mean change in scores was 3.4 ± 3.3, which was statistically significant at p < 0.0001.
An unexpected finding that participants did not directly record responses for was related to the collegiality and social interaction the interprofessional activity provided. Our observations were substantiated with informal feedback, photos and video indicating the students enjoyed the interactions with one another.
Three overarching themes were identified: (1) participants gained an appreciation and knowledge of other healthcare professionals’ roles, (2) participants gained an appreciation for the different healthcare professions’ contributions to client/patient care and (3) participants gained an appreciation for being respectful of other cultures, being prepared when travelling and knowing how to improvise while travelling abroad.
Providing students with opportunities to participate in interprofessional activities during their education can foster a more profound understanding of other disciplines’ roles in healthcare, increase awareness of and respect for different healthcare roles, and strengthen their collaboration and communication skills necessary to work with diverse healthcare professionals [28,29]. Activity Theory served as the theoretical framework for this interprofessional simulation activity. Figure 1 highlights the attributes of the framework as they relate to the activity.
Previous studies show that students participating in interprofessional education report increased confidence, improved attitudes towards teamwork and enhanced communication skills [8,10]. Interprofessional education is essential for strengthening future practice and optimizing client/patient outcomes and, as such, should be introduced while students are in their programs [8,30–33].
We used spring break as a theme for the interprofessional activity to encourage student interest and participation. Events that could occur while students are on spring break provided ideas for engaging and relevant scenarios. The spring break theme created a fun, interactive learning environment that may make learning more memorable. One objective for the interprofessional activity was to increase awareness and preparedness for adverse/preventable events that can occur over spring break, while another aim was to foster appreciation and respect for other cultures for students travelling abroad. Students noted they learned tips, practical skills and ways to be prepared when travelling, and importantly, they were reminded to be intentional to make an effort to respect the customs of other cultures. Travel opportunities can foster the development of cultural competence and global citizenship when students are aware and intentional.
Activity Theory stresses that learning occurs as students collaborate to achieve mutual goals and our simulation scenarios allowed students to actively engage with one another as they learned. Students learned about one another’s professions (skills, roles, workplaces) by actively working alongside one another. Exposure to the tools, decision-making strategies and treatment modalities used by each profession, combined with engagement and collaboration, made the learning more impactful.
Our findings aligned with work done by Battista, which indicated students learned as they engaged in simulated activities [17]. In our interprofessional activity, the students’ SPICE-R2 scores were statistically significant, and we gained a deeper understanding of what made the learning valuable. Students noted that they gained appreciation and knowledge of other healthcare professionals’ roles and their contributions to healthcare as they collaborated in the scenarios. Comments such as ‘I have a better appreciation of what athletic training education focuses on and how that enhances their job’, ‘I learned that athletic training students have good practical skills’ and ‘We are all great at different things, and it helps us to complement each other to improve patient care’ highlight the knowledge gained.
In addition to students benefiting from working with one another, the interprofessional simulation activity was designed and facilitated by a diverse group of faculty/community partners representing the many schools, programs and healthcare arenas. Their expertise led to the development of realistic and evidence-informed simulation scenarios and importantly provided faculty and community partners with an opportunity to get to know one another, socialize with and collaborate with other professionals in a fun, engaging activity. This may lead to future partnerships and interprofessional activities across the college and within the community.
Interprofessional education is an essential component of healthcare education as it has been shown to improve teamwork and enhance client/patient outcomes. As such, finding effective and impactful ways to introduce students to interprofessional practice during their education must be a priority for healthcare programs. In addition, despite barriers such as timing, scheduling and logistical planning, interprofessional education should involve both academic and community members to foster collaboration and optimize stakeholders’ expertise. Our interprofessional activity serves as one exemplar of how this can be achieved.
This study was conducted at a single academic institution using a small convenience sample; hence, the findings may not be generalizable to other institutions. In addition, the survey response rate was only 51%; thus, limited data may impact the interpretation of the findings. Based on the reports, it was clear that for future interprofessional simulations, more time is necessary for all activities and data collection.
Spring break is a wonderful opportunity for students to have a reprieve from their studies before the end-of-semester stretch. Facilitating interprofessional simulation activities prior to spring break is a novel approach to preparing students to stay safe while travelling. These opportunities allow students to learn from facilitators and one another about situations they usually do not discuss with others outside of their immediate friend circle. The simulation activities were intended to promote safety awareness, improve knowledge of managing adverse and/or preventable situations, enhance cultural competence development and provide a global perspective for students travelling domestically and/or abroad during spring break. Participating in such simulations provides students with diverse approaches to challenging situations.
Following participation in the multiple simulations, students reported learning about one another’s professions, appreciation for other healthcare professions’ roles, contributions of others’ roles to care, respect for other cultures and how to improvise during challenging encounters while travelling.
These interprofessional multi-simulation spring break activities could easily be replicated with students earlier in their educational journey, regardless of their major. It would benefit students to participate in these activities to prepare them for their first spring break as college students. Each specific simulation activity could also be offered independently of the others as stand-alone simulations. In addition, some of the activities may be adapted depending on the audience. For example, the ‘Yes, I can Say No’ simulation can be altered for medical students to prepare them for having difficult conversations with patients.
It’s essential to have a diverse planning committee when organizing an interprofessional simulation event. Each faculty’s unique lens can help view all the options and weigh the pros and cons to determine the best course of action. Having experienced facilitators at the interprofessional event is also a good idea to help the students understand its themes. Finally, have fun and get creative while planning an interprofessional simulation event, which will translate to the students and lead to a successful event with positive outcomes.
JV, SS, LHS, KG, TE, JP, SK, TA, AC-R, SF, ATM, NR, CD and JP (2) contributed to the conceptualization and successful implementation of project. JV, TA, AC-R, SS and JP contributed to the methodology. JP, TE, JV, MJP, TA and SS acquired and formally analysed the data. JV, SS, TA, LHS, SK, NR and ATM contributed to data interpretation. JV, SS, TA, LHS, SK, SF, NR, AC-R, ATM, MJP and KB contributed to writing and revising initial draft. JV, SS, LHS, KG, SF, TE, JP, SK, TA, AC-R, SF, ATM, NR, CD and JP (2) critically reviewed and revised the initial draft and all revisions. All authors approved the final version for submission.
This work was supported by two institutional internal grants: ‘Spring Break is Here! Swing into Spring Safely Simulations’. Sponsored by University of North Carolina Wilmington College of Health and Human Services Cultural Activity Grant. ‘Together We Make a Difference: CHHS Initiative for Interprofessional Collaborative Education and Practice’. Sponsor is the UNCW Applied Learning Strategic Initiatives.
None declared.
None declared.
The authors declare no conflicts of interest or disclosures.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.