
Access to and inclusion in simulation-based education (SBE) for remote and rural (RR) healthcare practitioners, irrespective of geographic setting, professional background and workplace context, is challenging. This challenge is compounded because simulation in healthcare education is acknowledged as a complex intervention, and healthcare systems are in and of themselves complex.
A realist review of published and grey literature was conducted, seeking to identify programme theories and to explore what works, how and why, in respect of mobile and distance SBE for healthcare practitioners in RR and harder-to-reach communities.
There is limited rigorous research in this field. Mobile and distance simulation programmes exist in physical, digital and hybrid forms. This makes simulation more accessible and inclusive for RR healthcare professionals in respect of facilitating simulation. It allows for clinical and simulation centres of expertise to collaborate with harder-to-reach communities enabling the contextualizing of learning with, from and about the needs of a target population. However, the challenges of implementing and sustaining mobile and distance simulation interventions are underexplored.
Mobile and distance programmes of SBE are introduced into and are subject to dynamic and heterogeneous social contexts. The intended outcomes of such programmes are dependent on building relationships, trust and networks between geographically distanced communities of practice. These social connections are the key mechanisms which support accessibility, inclusivity and sustainability. Further explorations of mobile and distance simulation innovations are critical to building capacity, sustainable solutions and enhancing future use.
What this study adds
Implementing simulation-based education (SBE) programmes can be complex [1,2] requiring careful attention to organizational contexts [3,4]. An exponential increase in SBE publications and empirical evidence advocates its benefits [5], yet few publications have focussed on exploring or explaining the implementation of SBE interventions in general, and far less in remote and rural (RR) healthcare communities. This research explored a simulation programme implemented in RR Scotland where, in common with other countries worldwide, there is inequity of access to SBE for healthcare professionals across geographical and professional boundaries [6,7].
Although Scotland is a small country, its population and healthcare workforce are unevenly distributed, geographically disadvantaging the highlands, islands and mainland RR communities [8]. The geographic distinctions of no bypass hospitals, remote, isolated and single practitioner islands convey the nuances of the challenges experienced with the provision of infrastructures and services for those living in and practising healthcare within these communities [8]. These challenges extend to healthcare education for staff where there is considerable variation in equity of access to clinical skills training, using SBE [7].
SBE is an embedded component of undergraduate, postgraduate and continuing professional education and training in healthcare professions curricula and workplaces worldwide [9]. The widespread adoption of simulation is underpinned by a growing body of published evidence affirming its benefits, supporting preparedness for practice, and improvements in patient safety and patient care [10]. However, the hegemony of SBE has emerged from hospital-based specialities, and bespoke simulation centres in academic or clinical locations [11]. Typically, SBE is adopted in strategic locations with geographic concentrations of simulation personnel, facilities and resources, which benefits convenience and cost for many and consolidates simulation faculty expertise and capacity [12]. However, many healthcare communities continue to face challenges connecting with and sustaining SBE initiatives [13,14]. This research explored an innovative programme aimed at addressing this challenge by implementing a mobile simulation facility, funded as part of a National Clinical Skills and Simulation Strategy by NHS Education for Scotland [15]. A key objective of this strategy was to provide high-quality SBE across geographical and professional boundaries. The Mobile Skills Unit (MSU) (Figure 1) was one element of the strategy and provides a peripatetic, versatile space for clinical and surgical skills education and simulation faculty development [7] and aims to promote accessible, inclusive and sustainable SBE for healthcare communities in RR Scotland [16].


The Mobile Skills Unit (photo courtesy of NHS Education for Scotland)
Health and social care staff living in RR Scotland report feeling professionally and physically isolated from clinical colleagues and specialities and some services [17]. These challenges impact upon the retention and recruitment of staff across the diverse RR healthcare contexts and workforces of NHS Scotland [18,19]. These issues are not unique but echo a global challenge for health professions education in complex healthcare systems [20]. Initiatives to promote new ways of providing health and social care and improve access to continuing education include UK national strategies [21,22] and international Global Policy recommendations for RR workforce development [23].
In RR communities such as in Scotland there is an acceptance of healthcare role and skill diversity and resilience [19] to address the tyranny of distance , the challenge of delivering healthcare in remote communities by heterogeneous healthcare teams [24,25]. This includes providing services for acute and chronic healthcare conditions, and the infrequent but urgent need to assess, stabilize and manage a critically ill or injured patient with limited resource, knowledge or skills until transfer to a tertiary care centre is possible. Training for these high acuity and low occurrence (HALO) events [26–28] typically means RR staff have to travel long distances. The time and cost of being away from home and work is inconvenient, but moreover may be prohibitive [25,29]. Recognizing these challenges, the National Clinical Skills and Simulation Strategy and the MSU were seen as proposed solutions to the ‘inequity of provision of high-quality clinical skills education using simulation’ affecting RR Scotland [7] (p.221).
However, Greenhalgh and Papoutsi argue that creative innovations which are designed to offer solutions and opportunities are complex to implement, with respect to their spread (replication) and scale-up (building infrastructure) [30]. This is particularly true in diverse social contexts such as in RR Scotland and other global contexts in which communities are harder to reach [2,31,32]. Therefore, this realist review was conducted as part of a longitudinal study and realist evaluation [33] and sought to explore the evidence base for SBE interventions targeting RR communities.
Realist methodological approaches to research are considered an appropriate theoretical lens when exploring the implementation of complex interventions within heterogeneous social contexts [34], and are advocated in health and social care and education research [35–38]. Realist reviews are a theory-driven, literature review methodology seeking to explore how complex interventions function in complex environments, pursuing an explanatory rather than a judgemental approach to expressing research findings [39]. Searching the literature during a realist review is iterative, creative, non-linear and continuous [40,41]. Figure 2 illustrates a comparison of a realist with a systematic review [42].

![Realist review compared to systematic review [42]](/dataresources/articles/contents-1710951602665-af16de17-d44d-4065-a0fb-3c382ccfc1ee/assets/porh1951f0002.jpg)
Realist review compared to systematic review [42]
Realist reviews seek a very broad range of evidence sources, not exclusively the peer-reviewed literature [32,43]. This is because realist reviews propose and test programme theories , which are the assumptions that stakeholders proposition about how and why interventions will work in practice [44]. Therefore, programme theories are the underlying unit of analysis for realist research [45]. Whilst, materially, interventions are comprised of the resources, activities, services, equipment and personnel offered to communities, in the realist research world, these combined tangible elements are considered programme theories. The underpinning principle of realist philosophy assumes that ‘Nothing works unconditionally in all circumstances’ [46] (p.126). Therefore, realist reviews typically ask the questions – what works, why, how, for whom? They ask: in what respects and circumstances, do interventions generate intended or unintended outcomes when introduced into diverse social contexts? Realist research seeks to explain the underpinning causative mechanisms [47]. Exploring contexts, mechanisms and outcomes is fundamental to realist reviews and evaluations.
Realist reviews like other literature review methodologies are guided by quality standards. The Realist And Meta-narrative Evidence Syntheses: Evolving Standards (RAMESES ) Project Quality Standards [41] was funded by the UK National Institute of Health Research’s Health and Social Care Delivery Research Programme. The RAMESES projects produced the quality standards and training materials for realist review and evaluation and informed this realist review: https://www.ramesesproject.org/media/RS_qual_standards_researchers.pdf.
Booth et al. [48] assert that an explicit and transparent reporting of the search logic counters the tensions between the creative realist and rigid systematic review protocols and demonstrates rigour consistent with realist inquiry. The six steps of a realist search and synthesis proposed by Booth et al. [48] guided the search logic adopted in this review (Figure 3).

![Steps of a realist search [48]](/dataresources/articles/contents-1710951602665-af16de17-d44d-4065-a0fb-3c382ccfc1ee/assets/porh1951f0003.jpg)
Steps of a realist search [48]
The guiding search question (step 1 ) was formulated in consultation with stakeholders and in accordance with the RAMESES Quality Standards [41] who advocate stakeholders are key informants in decision-making about the focus of the research, we asked: What does the published evidence say about the phenomena of mobile SBE in RR healthcare? Step 2, a background search and scope of published literature was followed by a review of stakeholder documentation (step 3 ) to identify initial programme theories and captured tacit and historical insights from these key informants [49]. Next, an iterative search for empirical evidence (step 4) explored a wider conceptual framework of simulation literature and innovative programmes targeting harder-to-reach communities. Step 5 , the testing and refining of initial programme theories, was conducted as part of a realist evaluation with empirical data collection [33]. This step is not reported in this publication; instead, this realist review documents and reports the realist search and synthesis (step 6) of the published literature identified.
Ethical approval was requested since this realist review involved stakeholder consultation and documentary analysis [38,41]. Ethical approval was granted by the University of Dundee Research Ethics Committee (UREC 16037).
The initial search of databases included the NHS Knowledge Network, Medline (via the OVID interface) and Google Scholar, adopting recommendations to use a restricted range of generic sources at this stage [39,50]. Medical Subject Headings (MeSH) controlled language terms and Boolean operators were adopted, minimal restrictions were applied and the search looked at a 10-year period (2005–2015), the time during which the MSU was proposed, designed and launched. In consultation with a librarian colleague [51], the following search terms were adopted:
(TITLE-ABS-KEY (simulation OR simulation-based) AND TITLE-ABS-KEY (“mobile clinical skills” OR “mobile learning lab” OR “mobile unit” OR “static unit” OR “mobile simulation” OR “mobile training” OR “mobile skills unit” OR “mobile surgical skills”) AND TITLE-ABS-KEY (clinical OR healthcare OR medical OR hospital* OR health OR nursing) AND TITLE-ABS-KEY (education OR course* OR training OR trainers OR educator* OR delivery OR programmes* OR pilot OR programme*)
Literature selection and appraisal were based on relevance (contribution to theory building) and rigour (data are credible and trustworthy), the key criteria by which literature is appraised in realist reviews [39,52,53]. Selection, appraisal and exclusion criteria were also guided by a Realist Review Appraisal Form from a publication by Jagosh et al. [54] to guide the identification of papers of relevance. Endnote reference management software was used for data extraction of published literature to organize citations, explore and analyse pdfs.
After screening and appraisal nine resources describing approaches to address the SBE needs of RR communities were identified. Three pertained to the MSU of this study [55–57]; however, one was excluded as this conference abstract proposed a qualitative research study which was not conducted. The remaining publications included an in-depth critique of an in situ intervention in the USA [58]; a descriptive report of a rural surgical bus in New Zealand providing education and mentorship to nursing and surgical staff remotely [59]; and a discussion of a UK-based clinical skills bus for undergraduate students [60]. A report for the World Organization of Family Doctors (WONCA) discussed case studies of clinical skills and SBE for RR practitioners, although it did not describe a mobile facility exclusively [25], and two papers reported surgical skills training specifically using mobile vehicles for simulation interventions [61,62].
Empirical research on mobile vehicles for simulation is lacking, and only one original research paper was identified amongst the eight reviewed, which were published between 2006 and 2014. The common focus of these mobile SBE publications was procedural skills acquisition, particularly HALO, acute and emergency skills and drills, and laparoscopic and minor surgical procedures. Learning opportunities were vaguely and varyingly described as facilitator-led and self-directed. The most frequently reported outcomes were learner satisfaction, and skills acquisition, which is typical of, but also a criticism of the quality and value of SBE publications [63–65]. What these papers shared were largely positive descriptions of SBE interventions, based on the reflections of participants and authors. They discussed creative and innovative solutions for engaging with SBE on-site rather than in a fixed simulation centre, thus making simulation more accessible and inclusive for RR communities in respect of the physical and/or human resources which facilitate SBE. However, none of the papers added to the literature on the sustainability of these interventions.
The nine papers analysed varied in their richness of descriptions of contexts and mechanisms, supporting the outcomes of the SBE programmes they advocated. Longer term outcomes of the interventions in respect of enablers and barriers were difficult to discern as none of the papers took a longitudinal view of the innovations they described. Common motives were driven by needs assessments underpinning the training for HALO events. Expressions of forging social connections, collaborative partnerships and informal networks within and across healthcare organizations, created opportunities to facilitate and capitalize on shared educational and physical SBE resources.
The search for programme theories (step 3) expanded on the background search to include programme documents via stakeholder consultation. These stakeholders were employees of NHS Education for Scotland, including the original architects of the MSU and staff responsible for its design, operationalization and facilitation of SBE. A large volume of programme documents included historic business plans, steering group meeting minutes, training needs analysis, annual reports, training records, course programmes and timetables, course feedback and evaluations from facilitators and participants and were shared in digital and paper formats.
During consultations, the social connections that were identified as causative mechanisms in the literature were also discussed and echoed by stakeholders who proposed that the MSU – works at the level of informal networks – and that supplying a mobile simulation vehicle alone was – a recipe for failure [66]. Seminal SBE publications have similarly asserted the fundamental need for simulation faculty development for specific educational and professional contexts [3,67,68] and argue that the inherent value of SBE is ‘unrealisable without skilled educators and technicians… and professional networks for simulation specialists’ [6] (p.5). The key mechanisms for implementing SBE interventions advocated by stakeholders are nurturing social connections alongside longitudinal faculty development to avoid a mere ‘train and hope’ [69] (p.6) approach to implementing SBE.
Stakeholder consultation and documentary analysis is recommended in realist reviews as a participatory way to identify authentic, contextually situated evidence [48]. Capturing the tacit knowledge and experiences of stakeholders narrowed and prioritized the focus of the study to three initial programme theories. These programme theories (Figure 4) are constructed as an if–then–because hypothesis, a realist research heuristic [49]. The reader may interpret this as – if we deliver a programme in this way (context) then this will bring about an improved outcome, because… (mechanism).

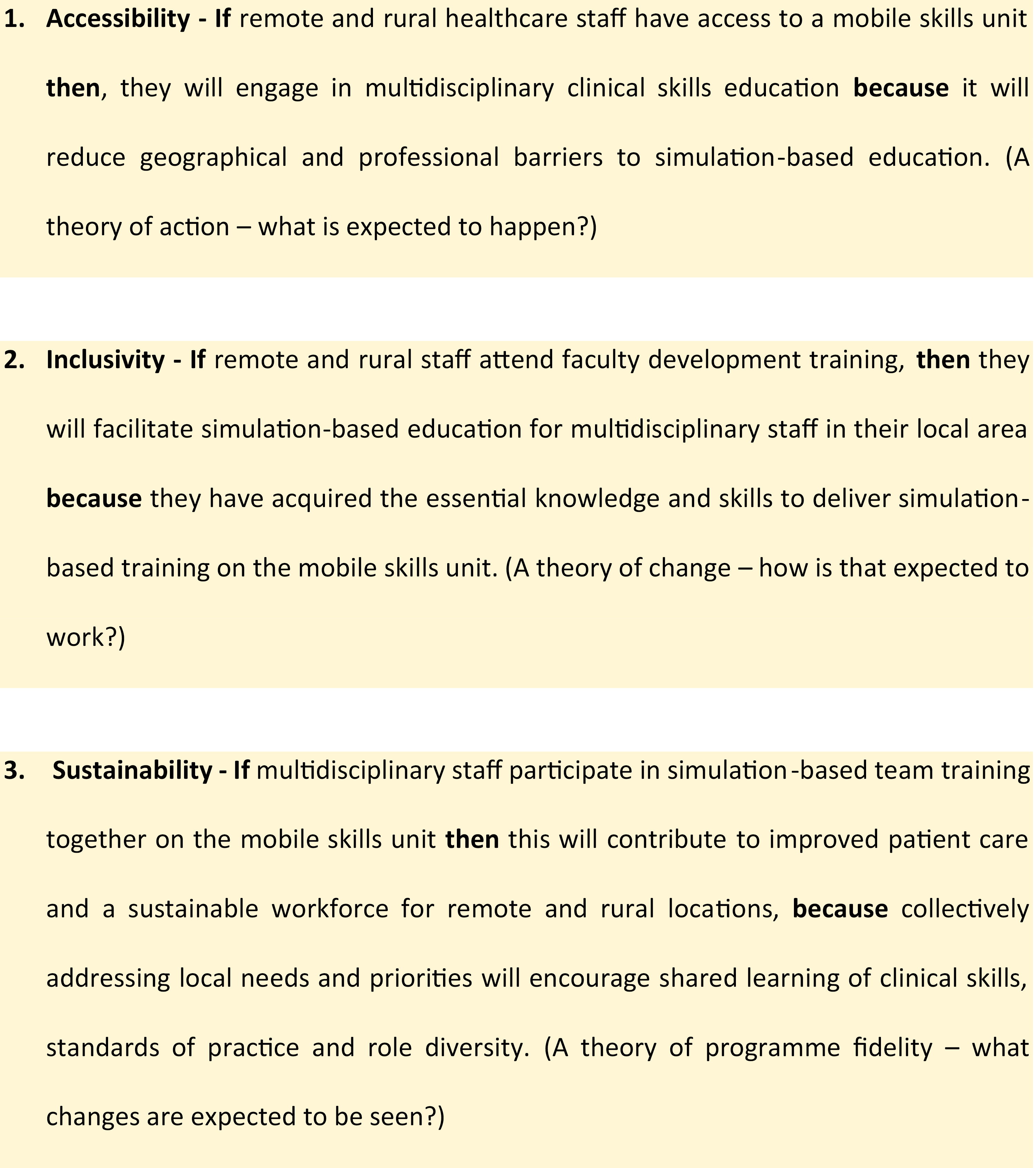
Initial programme theories (step 3)
Iterative strategies were employed to search for empirical evidence to test the programme theories proposed. This included additional database searches for published literature in Scopus, Web of Science and PubMed using the search terms above. In addition, search strategies included CLUSTER searching [70] (Citations; Lead author; Unpublished materials; Scholar searches; Theories; Early examples; Related projects), and ‘berry picking ; the foraging and browsing for information which is proximate to items of interest’ [48] (p.157). These complementary search strategies included exploring simulation journals for conference abstracts, library repositories for doctoral theses, ResearchGate for unpublished manuscripts, podcasts, webinars and Google for training courses or promotional materials. The rationale for this unconventional searching approach is advocated by the RAMESES Standards [39]. The purposive iterations of searching pursued titles and abstracts if they implied aspects of mobile or distance simulation, but not exclusively describing a mobile vehicle. Date restrictions were not applied during iterative searching; the oldest paper identified was from 2004 and the last was in 2020 when the search concluded.
After screening and appraisal of publications and grey literature, three mobile simulation typologies and five simulation programmes were considered of relevance. The iterative searching identified publications which have in common the concepts of hub and spokes [71] and outreach [72], programmes seeking to make simulation accessible and inclusive to harder-to-reach communities. Whilst the initial focus of this research was an exploration of the MSU, a physical unit, this is an example of ‘a family of programmes’ [73] (p.25) of mobile and distance approaches to simulation. It is a fundamental aspect of a realist review to seek relevant literature which identifies programmes in diverse contexts, with variable outcomes so as to explore the reasons (the causative mechanisms) for what, how and why they work (or not). The iterative searching strategies and metaphorical zooming out and in [74] of the literature created the opportunity to illuminate and magnify [75] a body of evidence of contrasting simulation interventions, identifying key features, variables and relationships between heterogeneous simulation phenomena [67].
The term mobile simulation is defined by the Healthcare Simulation Dictionary as mobile in the digital sense, inferring simulations with minimal or no equipment, such as tabletop, or computerized modalities without manikins and in the portable sense, a physical simulator that can be moved, operatable with or without power cords or communication cables [76]. Mobile simulation enables access to SBE opportunities by removing or restricting distance-orientated barriers and generating point-of-care, in situ simulation (ISS) opportunities [77]. This may be in a transient environment such as a large mobile vehicle, or the use of mobile cart situated within or shared between institutions, or transport and delivery of part-task simulators [77].
Distributed simulation (DS) intends to create simulation opportunities which are on-site, real enough, near enough, flexible, practical and low cost. Kneebone et al. argue that the widespread adoption of SBE will not be realized unless innovative solutions acknowledge barriers to multi-professional access [11]. The original concept of DS used an inflatable tent-like surround, to represent an operating theatre, using local equipment, and images of a clinical space. This aimed to minimize the restrictions of access to fixed-site simulation centres, the organizational limitations of in situ opportunities and the predominance of medical speciality-focused simulation activities. DS has been validated in the UK in a tertiary hospital setting [78] and a district general hospital [79] however, no publications beyond these were identified describing DS. The evidence for DS confirms accessibility and inclusivity reducing barriers for some, but as a mobile simulation concept or terminology, the evidence of sustainability is limited.
ISS is very widely reported as a learning event conducted in the real clinical environment [80]. ISS allows the participation in and observation of everyday or atypical activities and behaviours of healthcare professionals (HCPs) [81] to introduce, develop and test existing or new practices, procedures and systems [82] such as those rapidly introduced during the COVID-19 pandemic [83]. Examples of ISS demonstrate the effectiveness of SBE for improving patient outcomes through translational simulation [84], for example with multi-professional staff in obstetric departments, standardized educational materials and faculty development [85–87]. However, the empirical evidence also reports that individual and team knowledge and skills can be learned equally well in ISS, on-site or fixed simulation centres, whereas organizational learning is most suited to ISS [85,88–92]. The purpose of, rather than the setting for, simulation is key to achieving intended outcomes [88,93,94]. Aspects of ISS were restricted by COVID-19; however, publications emerged describing ISS in response to COVID-19, recognizing its value for individual, team and organizational learning, developing and refining new and safe approaches to clinical skills practices, and diagnosing human and organizational latent safety threats [83,95,96]. ISS is an established mobile simulation typology, giving rise to the use of simulation as the focus of and an instrument for researching organizational learning and sociocultural experiences [97,98]. The wealthy continuum of evidence and diversity of ISS supports the notions of making ISS accessible, inclusive and sustainable.
Based on the concept of telemedicine, telesimulation, telefacilitation, telementoring and teledebriefing use digital and technological solutions to create social connections for remote participation in SBE [99]. Telecommunication and simulation resources used together provide largely synchronous education, training or assessment at distant locations with specialist clinicians or more experienced simulation faculty, supporting remote colleagues [27,99]. Telesimulation descriptions vary according to faculty–student ratios, types of simulation conducted and the degree of involvement of the facilitating versus remote site [100]. The literature describes applications of the use of telesimulation for procedural skills learning [101], surgical skills [102], scenario-based training [103,104], simulation-based assessment [13] and interprofessional education [99]. The use of both a physical mobile unit and telesimulation to deliver procedural skills training provided expert mentorship for simulation facilitators, overcoming barriers including cost and distance to delivering SBE in RR locations [27]. An experimental study taught and assessed approximately 70 medical students in the insertion of surgical chest drains using telesimulation for procedural skills simulation with expert mentorship, overcoming geographical barriers to SBE in RR communities [27]. Globally democratizing SBE through technology is a notion promoted by Ahmed [105] who reports digital and technology-based solutions including successful live streaming of both simulated and live surgery for educational purposes between centres of excellence and developing countries. As a modality, telesimulation has increasing currency as the simulation community expands and learns from responses to the pandemic and generates creative ways to facilitate access to simulation within physical centres and support communities constrained by access to and transport of simulation faculty and equipment [106–108]. The pandemic has created an impetus to advance synchronous and asynchronous forms of flexible learning [109] increasing the potential for creating accessible, inclusive and sustainable formats of telesimulation.
The INSPIRE simulation network describes an innovation involving flying faculty from a North American centre of paediatric expertise commuting to regional community hospitals who have limited opportunities for SBE [110]. This simulation intervention known as the Community Outreach Mobile Education Training (COMET) programme embraces the three typologies of mobile (portable), distributive and ISS described above and was developed to enhance the confidence and skills of community-based staff in responding to HALO paediatric emergencies. It closely aligns with the aforementioned key mechanisms of creating meaningful community-based partnerships, facilitating the communication of best practice, and distributing up-to-date policies, education and training, providing opportunity for system testing at these community sites [110]. A particularly revealing causal insight expressed by the authors is that of a professional courtship [111] which has been key to relationship building and developing trust between the hub and spokes. The sharing of expert knowledge and nuances of specialist clinical management are combined with an appreciation of local contexts aimed towards an improved level of paediatric care in rural communities. The forging of interpersonal connections and mutual respect for colleagues is key to enhancing the translation of learning from simulation experiences to changes in clinical practice. Framing simulation courses as quality and safety initiatives over and above educational opportunities has been key to securing local buy-in and the sustainability of this programme. A notable outcome was an increase in patient referral patterns post simulation courses, attributed to the connections forged and increased awareness of the benefits of early contact with tertiary centres [110]. The COMET programme proposes a longer-term sustainability goal of upskilling locally based clinical staff as future faculty to support participation in and dissemination of the COMET programme enacted through a community of practice.
A Neonatal Outreach Simulation (NOS) programme illustrates the notion of hub and spokes for small rural hospitals in two settings in the USA and Canada which have a low frequency of neonatal deliveries [112]. Acknowledging similar simulation-based life support courses, the authors consider the unique feature of NOS as the longitudinal, interprofessional and in situ nature of the programme. This enables crucial relationship building between the hub and the spokes locations in respect of HCPs who work in rural communities (inclusivity) and the medical emergency retrieval services who deliver training and support, developing simulation faculty apprenticeships (sustainability) among local colleagues [112]. Two diverse centres are hosts of the NOS programme, having adapted the NOS programme for their own contexts (accessibility) via needs assessment to define and support local requirements using Kerns six-step approach to curriculum development [113]. An Indiana-based programme welcomes a flying faculty with simulation resources when required, whereas due to the vast distance constraints, a Yukon example engages in NOS through telesimulation. The latter example describes the Yukon’s centre as having all the physical simulators needed for delivering training but requiring NOS as the motivational dimension to trigger regular engagement in a programme of SBE. This is inferred as a key causal mechanism to invigorate locally based training to take place. The collegiate partnerships which developed supported quality improvement efforts and patient care practices (outcomes), within a context where multiple stakeholder engagement provided practical and financial support, and local commitment and investment in the NOS programme afforded protected time to release staff for training [112].
Sustained clinical skills proficiency and patient safety outcomes have been demonstrated using outreach and minimal technology through the global training programme Helping Babies Breathe (HBB) [114]. This is an early example of programmes aiming for widespread implementation across low resource settings in Asia and sub-Saharan Africa to address WHO Millennium Goals [115,116]. Two systematic reviews of the HBB interventions described strategies which support the proposed outcomes of these programmes, including physical simulation resources to facilitate psychomotor skills training. However, these physical resources are not described as the key mediators for skills acquisition, effective and sustained learning in these low-resource contexts [116]. The causal mechanisms are attributed to resources such as peer-supported coaching, mentoring, assessment of skills and refresher practice which resulted in increased confidence leading to sustained local impact from the programme [116,117]. Although widely adopted, HBB has been criticized for improving simulated performance but not the clinical management of neonatal patients or perinatal mortality [118]. It is argued this is due to a lack of embedding HBB opportunities beyond the hospital setting, despite most of the perinatal and neonatal morbidity and mortality occurring in community settings [116,117]. Opportunities for high-frequency skills practice, skills maintenance and testing in community healthcare contexts are limited in low-resource settings, and hence a barrier to accessibility and inclusivity of sustaining the HBB programme beyond the hospital setting [119].
The opportunities and challenges of sharing SBE courses, resources and instructional materials between academic institutions, and investment in infrastructure to ‘facilitate downstream cost savings’ is reported by Laack et al. [120] (p.1), aiming to widen access to SBE and mitigate against barriers to implementation across academic institutions, states and continental boundaries. This programme of SBE was implemented, evaluated and enhanced in respect of interprofessional collaboration. It aligns with a seminal Lancet report which advocates ‘linking together through networks, alliances, and consortia between educational institutions worldwide’ [20] (p.1) to transform and strengthen education in low-resource health systems. This mixed methods study discussed the feasibility, benefits and challenges of sharing SBE courses across institutions, and the authors emphasized the need for consideration of local culture, context and needs when sharing resources and implementing programmes in distinctive institutions [120]. They identified that the considerable upfront costs of establishing the programme were offset by being a one-time outlay spread over time and institutions. The advantages described were cost and time saving for clinicians and faculty and were considered compelling motivators for sharing SBE courses. The planning and infrastructure building between the hub and spokes was felt to have potential and promise; however, in practice the outcomes were not fully realized in this pilot stage of implementation despite early lesson learned, and thus evidence of longevity and sustainability is limited.
The last mobile programme discussed is the NHET-Sim programme, a national strategy aiming to fulfil a need for accessible, inclusive SBE and sustainable faculty development across Australia [121]. The programme recognizes and seeks to address the challenges of simulation resource duplication, inconsistent facilities utilization, discipline-specific silos, and the intersection of academic institutions and health services sectors [121]. This government-funded directive stipulates that 25% of the NHET-Sim programme should focus on ensuring outreach to healthcare staff in RR settings, realized as distance learning and in-person education and training. Like the COMET programme, NHET-Sim encourages peer exchanges and the development of resources including locally contextualized scenarios which provide discussion opportunities about the challenges of working in smaller teams with limited resources. In turn this generates outcomes such as facilitating conversations about when and how to engage with medical retrieval colleagues to transfer patients to tertiary care. In this interprofessional context a simulation community of practice emerged, with a critical mass of participants, and shared language of SBE. Remotely connecting entry-level and emergent simulation education cultures with specialized simulation education support at a central hub, emanates accesibility and inclusivity. These strategies across local, regional and national levels created rapport and repeated opportunities for practice, knowledge exchange and scholarship. The authors assert that these hub and spokes and outreach forms of simulation were implemented to engage new groups of potential participants, and were anticipated to be more responsive to local needs because co-facilitation and learning took place in situ [121]. Nevertheless, this was not without challenges. Local resistance to buy-in and other competing priorities threatened the infrastructrual scale-up and sustainability of support for locally based facilitators [121]. Implementing SBE programmes is complex, and there is added contextual complexity in the RR setting where one-size does not fit all contexts [25]. However, this Australian national strategic approach, with a focus on sharing simulation expertise and resources, resulted in a network of widely distributed faculty. This community of practice promotes accessible and inclusive simulation and in turn enhances local buy-in, ownership and participation, the causative mechanisms for sustainability [121].
Realist reviews do not intend to conclude a net effect that interventions work or not. Rather they explore heterogeneous interventions and modalities to illuminate and magnify phenomena of interest [75]. The concept of mobile simulation exists in idiosyncratic physical, virtual and social forms, with the intention of enabling simulation opportunities and overcoming distance and/or resource-orientated barriers. Moreover, it enables the contextualizing of learning with, from and about the specific needs of a target population, providing clinical and simulation expertise in harder-to-reach communities. The challenges of accessibility and inclusivity in SBE are addressed by the simulation programmes described in this review; however, there is less evidence of the sustainability of such innovations across diverse infrastructural contexts.
Realist research asserts that interventions or programme theories are not implemented into a social vacuum and encourages researchers to explore the social architecture in other words – the structure and agency of a context to explain the mechanisms of how, why and for whom intended outcomes are achieved, or not [73]. Implementing programmes of mobile and distance simulation manifests in the tangible form of equipment, personnel and combinations of these and other resources into heterogeneous social contexts. These are the visible, observable and measurable outcomes of any SBE interventions which are compared here with the image of the tip of an iceberg (Figure 5). Explaining how and why these observable outcomes emerge requires a deeper exploration of social contexts, to explore the causative mechanisms. In other words, what motivates and triggers support, or conversely which barriers inhibit intended outcomes? These findings may be hidden below the metaphorical waterline.

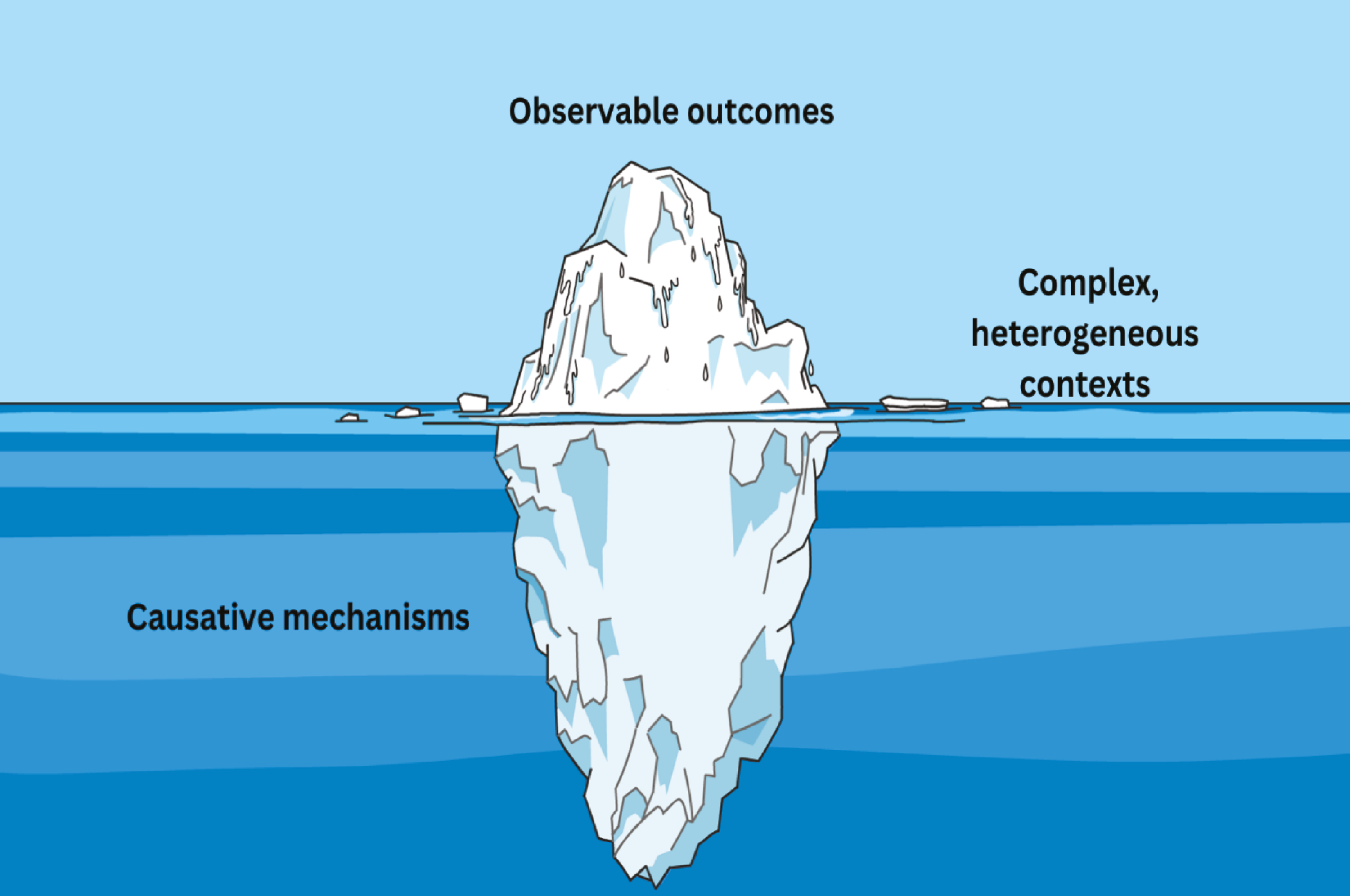
A realist iceberg analogy (edited in https://www.canva.com/)
Social contexts are the complex, dynamic backdrop for the adoption of any intervention, which in turn becomes the product of its context [49], and so simulation stakeholders may assume that a proposed intervention (programme theory) offers innovative solutions to perceived challenges, generating learning and improvement. However, while observable outcomes may be highly visible and easy to make an early judgement about, they may also be transient and maladaptive in different contexts and may not support sustainable intentions.
The literature described in this realist review reveals a heterogeneity of interventions and contexts, and the intended outcomes are attributed to the strength of relationship building, social networks and connections which are the causative mechanisms resulting from insightful implementation approaches within the co-located communities of practice. This realist review proposes that the scale-up (infrastructure building) of SBE interventions is more socially and contextually contingent than dependent on the spread (replication) of its physical resources and environments [29].
The strengths of this realist review are that it showcases to the simulation community a methodological approach for researching SBE using realist theory-driven approaches. It seeks to acknowledge, explore and advance our understanding of complexity in relation to the implementation of simulation interventions. This publication responds to calls for research which adopts theory, innovative methodologies and methods to study simulation for health and social care [65] and therefore contributes valuable knowledge to the Healthcare Distance Simulation Collaborative [122]. However, a limitation is that this realist review was conducted prior to the characterization of the Healthcare Distance Simulation Collaborative, and hence this concept was not identified as a search term during the review. This Collaborative has since generated much needed new evidence [122], and guidelines [123] as well as creating a nascent research and practice community [124] for the advancement of SBE for harder-to-reach communities. New evidence published subsequent to this review [125] also provides this community with rich and varied insights into mobile and distance simulation programmes. This realist review may now be a valued contribution to integrate with developing evidence-base of the Healthcare Distance Simulation Collaborative.
This realist review of mobile, distance, outreach, and hub & spokes programmes explored heterogeneous examples of simulation interventions. These simulation interventions provide improved geographical access and professional inclusivity for some RR and harder-to-reach communities. However, the longitudinal evidence of sustainability is limited, and against a backdrop of global conflict, of human, health, environmental and financial constraints, increased access, inclusion and sustainability are vital yet are arguably increasingly uncertain. Implementing SBE interventions is complex and non-linear, and more longitudinal sociological research is needed to explore and explain what works, for whom, in what circumstances, how, why and in what respects?
Grateful thanks to Dr. Sean McAleer, for his time, kindness and critical reading, also, to Mr. Scott McGregor, librarian at the University of Dundee.
Susan Somerville designed and conducted this research as a PhD candidate and was supervised by Stella Howden, Jean Ker and Susie Schofield. The manuscript was written by SS and critically reviewed by the co-authors.
NHS Education for Scotland (NES) funded this PhD study.
None declared.
Ethical approval was granted by the University of Dundee Research Ethics Committee (UREC 16037).
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
83.
84.
85.
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.
102.
103.
104.
105.
106.
107.
108.
109.
110.
111.
112.
113.
114.
115.
116.
117.
118.
119.
120.
121.
122.
123.
124.
125.