
The ASPiH Standards 2023 provide a common framework within educational and healthcare sectors, bolstering quality assurance for simulation providers, regulators, professional bodies and commissioners. They endeavour to meet the current needs of simulation practitioners and learners, reflect the evolution of simulation practice, and account for emerging technologies. Therefore, they are applicable to any modality of simulation-based education and training as well as to translational and transformative simulation interventions, including the use of simulation for quality improvement processes, whether carried out at education centres, simulation facilities or at the point of care.
The standards encourage adherence to core values of safety, equity, diversity and inclusion, sustainability, and excellence. They provide guidance for all simulation practitioners, highlighting key principles for planning, facilitation and evaluation of simulation activities, as well as recommendations for optimum resource management.
Implementation of these standards will require consideration of how they apply to each individual context, and what outcome measures are most meaningful to demonstrate alignment.
The Association for Simulated Practice in Healthcare (ASPiH) is a learned body that focuses on the development and application of simulation-based practice in health and care contexts. Based in the United Kingdom, it has a worldwide membership. It is a not-for-profit organization bringing together multi-professional representatives drawn from higher education, clinical practice and academic disciplines allied to health and care. It aims to improve the safety and quality of care provided to patients, as well as staff well-being, through the practice of simulation.
The ASPiH Standards were first published in 2016, describing the attributes required to design and deliver effective simulation-based education and practice. Since then, they have provided a common framework within educational and healthcare sectors, and underpinned quality assurance for simulation providers, regulators, professional bodies and commissioners.
In November 2021, ASPiH initiated a formal review and an update of the framework, aiming to meet the current needs of simulation practitioners and learners, reflect the evolution of simulation practice, account for emerging technologies, and address themes such as interprofessional simulation, sustainability, equity, diversity and inclusion. The revision process has included a literature review, ample consultation through virtual and face-to-face meetings, analysis of contributions, drafting of the revised standards and peer review by international simulation experts, as well as stakeholder discussions and a member survey capturing perspectives on the proposed draft (Figure 1) (Figure 2).

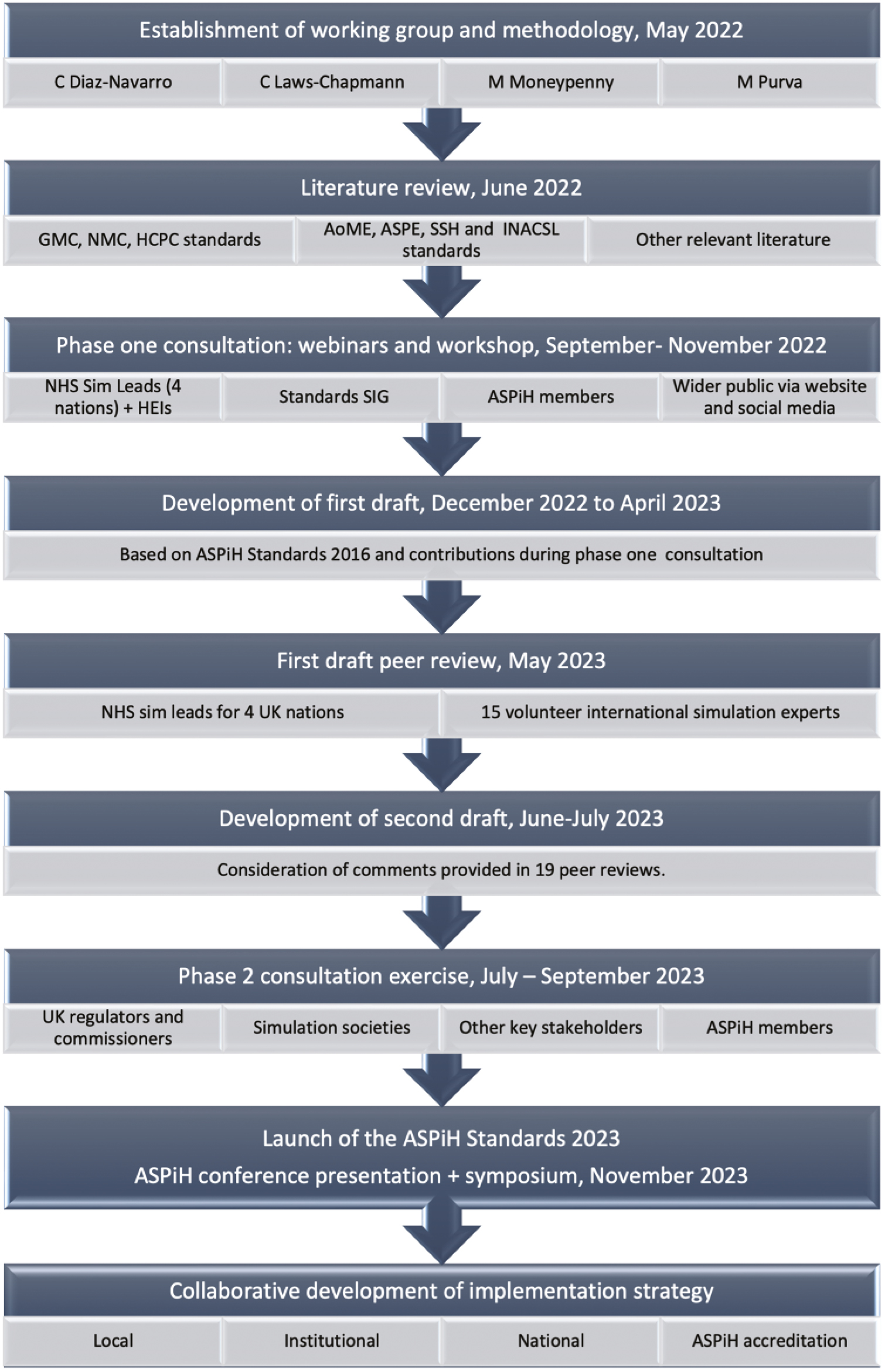
Development process for the ASPiH Standards 2023.

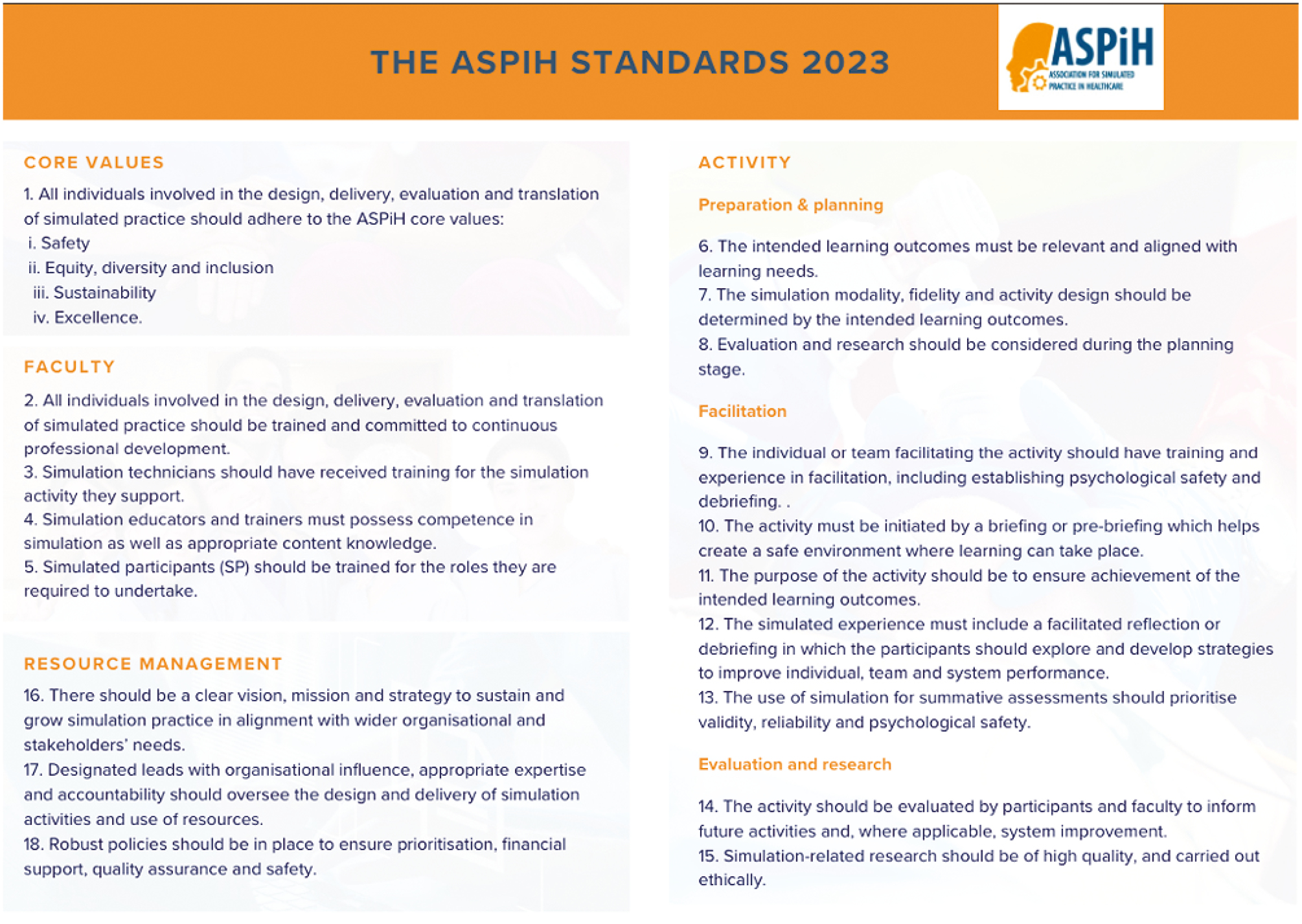
The ASPiH Standards 2023.
The revised ASPiH Standards continue to focus on elements and principles of theory and evidence-based practice applicable over the broad spectrum of simulation in health and care as a guiding compass for decision-making as an educator.
The standards are applicable to any modality of simulation-based education and training as well as to translational and transformative simulation interventions, including the use of simulation for quality improvement processes, whether carried out at education centres, simulation facilities or at the point of care. The principles included in these standards are formulated broadly so that they are useful when considering innovative approaches or emerging technologies. We expect these standards to continue to develop and evolve in line with developments in the field.
The implementation of these standards will require consideration of how they apply to each individual context, and what outcome measures are most meaningful to demonstrate alignment. ASPiH is committed to working with institutions and individuals to support the development of implementation strategies, as well as continuing to provide accreditation opportunities.
We use the term ‘simulated practice’ to refer to the complete array of structured activities that represent actual or potential situations in education and practice, which allow participants to develop or enhance their knowledge, skills and attitudes, or to analyse and respond to realistic situations in a simulated environment [1].
We refer interchangeably to ‘simulation practitioners’ (including technicians and simulated participants [SP]) as faculty, and to ‘simulation participants’ as learners; these terms comprise individuals involved in pedagogical and non-pedagogical simulation, such as activity for the purpose of innovation or improvement.
We have chosen the phrase ‘health and care’ in order to include any care settings that might benefit from simulated practice such as primary care, hospital and prehospital services, mental health, community, and social care.
We acknowledge the limitations to this framework: Whilst we provide practical and broad recommendations to address the issues raised during the consultation process, we are aware that further work is required to define more detailed standards for simulation-related research. Notably, it is not the remit of this document to explore the many modalities of simulation currently in use, from the more traditional psychomotor skills training, manikin-based scenarios, hybrid simulation or SP to tabletop simulations, cadaveric simulation, telesimulation, the use of avatars, or extended realities.
This work has been carried out by volunteer members of the ASPiH standards working group and peer reviewers. No funding has been received to support this work. The authors have no conflicts of interest to declare.
We hope that the application of these standards will support learners, simulation practitioners and wider organizations, bolstering patient safety in benefit of patients, service users, families and communities.
Simulated practice should support and advance high-quality and ethical health and care provision and nurture patient safety [2–4]. This requires simulation practitioners and participants to demonstrate their professional integrity, including attitudes and behaviours that hold patients, service users, learners, co-workers, departments and organizations in high regard [5].
The ASPiH core values have been developed based on broad consultation with the international simulation community and cross-referenced with available evidence. They should be promoted by simulation practitioners, embedded within simulation networks and organizations, and permeate the process of design, delivery and evaluation.
Standard 1: All individuals involved in the design, delivery, evaluation and translation of simulated practice should adhere to the ASPiH core values.
All simulation activities should be safe.
Safety encompasses physical and psychological aspects relating to simulation participants and practitioners, as well as the safety of patients, service users, and the wider health and care system [6].
Consideration must be given to the physical safety of all participants in simulation activities. For example, there may be a risk of injury by sharps, manual handling of heavy objects, unsafe defibrillation, contamination by animal products, or use of simulated or expired drugs in care areas.
It is incumbent on simulation practitioners, participants and anyone else involved in the simulation activity, to understand and minimize the risks to physical safety [7–9]. Notably, when delivering in-situ simulation, special consideration must be given to ensure the safety of patients, staff, the organization and the wider public [10].
Psychological safety is ‘the belief that one will not be punished or humiliated for speaking up with ideas, questions, concerns, or mistakes, and that the team is safe for interpersonal risk taking’ [11]. Psychological safety is essential for effective facilitation and learning, and it needs to be created and maintained throughout simulation planning, activity and evaluation [2,5,12]. This may include upholding explicit fundamental principles such as ‘we believe that everyone participating in activities … is intelligent, capable, cares about doing their best and wants to improve’ [13].
Mutual respect must be at the core of any health and care simulation activity as it enables faculty and learners to co-create a safe psychological and learning environment [5,12]. This psychologically safe environment has positive effects on both engagement with and learning from a simulated activity.
All people involved in the design and delivery of simulation-based activities should adopt a person-centred approach, adhering to equity, diversity and inclusion (EDI) principles for learners, faculty, staff, patients, service users, carers, families and communities.
Being person centred in simulated practice requires a focus on the needs of the individual [14]. This means that the preferences, needs and values of all participants inform the activity which, in turn, supports mutual respect [5,12].
All individuals taking part in simulation should conduct themselves in a manner that adheres to the four principles of biomedical ethics: autonomy, beneficence, non-maleficence and justice [2,15,16].
People involved in the development of simulation should work collaboratively, ensuring equitable and respectful co-production with patients, service users and staff representatives linked to the learning outcomes [17]. Cross-system partnerships should be established to evolve approaches, share knowledge and expertise, and proactively develop equity of access across professional groups, departments and organizations.
Simulation facilitation should, where possible, include an interprofessional faculty and consider equity, diversity and inclusion in relation to learners, faculty, staff, patients and service users [18].
EDI experts should be consulted and included in the design and delivery of simulation, particularly when the activities seek to address EDI issues. Continuing professional development on EDI should be part of any simulation faculty development programme.
Simulation activities should be designed sustainably regarding content, design and delivery, utilising resources efficiently and with consideration for the ecological impact of all aspects of simulation practice.
Climate change was declared as the greatest threat to global health in 2009 [19]. Global environmental changes affect us all, not only across professions but worldwide [20]. In order to reduce greenhouse gas emissions and carbon footprint, it is essential that health and care learners and staff are equipped with the knowledge, skills, values, competence and confidence they need to sustainably promote the health and well-being of current and future generations, whilst protecting the health of the planet [21,22].
Many activities of health and care education and provision, including procurement, energy and water demands, and generated waste have the potential to contribute to global greenhouse gas emissions [23].
Simulation practice should include sustainability considerations regarding their inclusion in learning objectives and outcomes when relevant, as well as in relation to efficient use, safe reuse, procurement, sharing, and appropriate disposal and recycling of resources.
Sustainability includes the provision of effective simulation and translation of learning into individual and team behavioural change as well as system design, adaptation and improvement in health and care. It also includes the development and maintenance of resilient simulation practitioners and participants, who support one another and nurture progression for all staff [24].
Simulation practitioners and organizations should strive for excellence through planning, reflection, research and evaluation, thereby leading to continuous improvement of all aspects of simulation practice in health and care.
Simulation planning and practice should be evidence-based and must fulfil the needs of the learners and any other participants, as well as health and care institutions and systems, aligning to relevant wider curricula and regulatory bodies’ requirements [25].
Simulation practitioners should embrace individual and shared reflection as a way to continue to learn and improve throughout their professional careers [26,27], and model this behaviour into their simulation practice [28,29].
Evaluation of the simulation activity allows the assessment of the effectiveness and impact of training and is crucial to capture and share best practice [30].
Quality assurance and continuous quality improvement are essential for achieving excellence and can be aligned to meeting standards, fitness for purpose, achieving institutional goals or fulfilling learner needs [31]. Any of these perspectives requires clarity in planning and targeted evaluation.
Current simulation practice transcends the sphere of education and training, and includes simulation activity with the purpose of understanding and improving care, mitigating risk and reducing error, as well as analysing and testing health and care systems [32,33].
These standards refer to simulation practitioners as ‘faculty’, and include under this term technical personnel, SP, educators and trainers. This section provides standards of best practice for all those who are engaged in the design and delivery of simulation-based practice.
However, specific qualification requirements may be regulated by national and institutional contexts.
Standard 2: All individuals involved in the design, delivery, evaluation and translation of simulated practice should be trained and committed to continuous professional development (CPD).
Faculty may include individuals with experience in simulation-based practice, content experts in the subject being delivered or both. It is essential that faculty who are designing, delivering or debriefing in the context of simulated practice should be appropriately trained in the methods and resources being used [34–37].
This training should include, at a minimum, the following competencies:
– Provision of a safe learning environment, with particular attention to psychological and physical safety for participants, faculty, patients and service users [2,7] [core value (cv) I].
– Promotion of equity, diversity and inclusion within the design and delivery of simulation, and prevention of harm to participants and faculty as a consequence of behaviours such as tokenism, misrepresentation, stereotyping or microaggressions [38,39] [cv II].
– Competency in debriefing, as this is a critical component of simulation-based practice which encourages shared reflection and facilitates learning [34,35].
– Application of relevant up-to-date Human Factors and Ergonomics knowledge, including concepts such as Safety ll, socio-technical systems, quality improvement, as well as social and cognitive skills [40–42].
Standard 3: Simulation technicians should have received training for the simulation activity they support.
Simulation technical personnel are often essential in the delivery of quality-assured simulation-based activity, and should be trained and supported to achieve appropriate professional recognition. Whilst there is variation in their responsibilities, their specific role should be well defined, and include core knowledge in technologies and methods used in the planning, preparation, and execution of simulation-based health and care activity [43].
All technical personnel should have a regular performance appraisal, and be supported to attend training and engage in CPD activities required for their role [44].
Technicians should be encouraged to contribute and innovate, to increase the quality of simulation-based practice and potentially contribute to return-on-investment [45].
Standard 4: Simulation educators and trainers must possess competence in simulation as well as appropriate content knowledge.
Competence in simulation and appropriate content knowledge may be achieved either by subject matter experts with training and experience in simulation design and delivery, by simulation practitioners with appropriate content knowledge or by simulation experts and content experts teaming up, working together in ensuring that the activity produced is conducive to reflective learning.
Collectively, individuals involved in the design and delivery of simulation must be able to:
– apply appropriate simulation modalities and educational methods to simulation design and delivery, considering relevant standards and expected competencies applicable to each profession involved in the activity [34]
– engage in reflective practice, meta-debriefing and evaluation of faculty performance by learners and peers, which should be integral to simulation practice [46,47].
Additional considerations for novice faculty include:
– An introductory course (or courses) should expose and orientate novice simulation faculty to the principles of adult learning and explore underpinning educational theories relevant to the spectrum of simulation [48].
– Specific training in pre-briefing, briefing, facilitating simulation and debriefing should be provided to new faculty, as debriefing is recognized to be the most important element of learning in the simulated environment [34].
– New faculty should observe or co-facilitate simulation activity alongside a more experienced faculty member and receive feedback using validated tools [49,51].
Faculty delivering human factors training should have undergone training (or equivalent) in systems engineering, human factors or other systematic approaches to optimising system performance, staff well-being and patient safety [50].
Faculty development is a lifelong process and should be supported by mentorship wherever possible, and regular performance reviews.
Faculty should engage in CPD activities recognised by the individual’s professional body [36], such as courses, conferences, academic activities and regular appraisal of literature [46]. A record of these CPD activities should be maintained.
Standard 5: Simulated participants should be trained for the roles they are required to undertake.
Any faculty member (whether an actor or otherwise) portraying patients, service users, family members, or health and care professionals in simulated practice should be cast according to EDI considerations, and trained with regard to the role they are expected to play in the activity (including providing feedback or debriefing if applicable), in line with specialist guidance for best practice [52].
The term ‘activity’ is considered to encompass any event, or series of events, which use simulation as a technique for learning, assessment, improvement or research.
Simulation participants are interchangeably referred to as learners, as there should be learning out of any simulation activity.
In these standards, intended learning outcomes (ILOs) include those achieved through assessment, research and quality improvement activity.
The following principles are applicable to any simulation modality, from procedural skills training, to in-situ, cadaveric, tabletop, remote or extended reality simulation.
In order to adhere to the four principles of biomedical ethics (autonomy, beneficence, non-maleficence and justice [2,8,9] [cv II], all simulation activities should strive to be free of commercial bias, in particular, that which may arise from funding. Declarations of conflicting interest are encouraged in all cases where external funding sources or collaborative relationships with suppliers are or have been present, or where there could be a perception of a conflict of interest of any kind.
Standard 6: The ILOs must be relevant and aligned with learning needs.
For the purpose of these standards, the term learning outcome encompasses ‘learning’ in the broadest possible sense, and includes gaining new knowledge in the context of system improvement, public engagement and research.
The ILOs must be designed taking into consideration the needs of the participants and those of the wider health and social care system, including patients and service users [34,36,46,53–55].
Whenever multi- or interprofessional activities are designed, the ILOs should be co-designed by representatives from the involved professions, and should align with the needs of each staff group.
Simulation participant needs may be ascertained by referring to a relevant curriculum, or by carrying out a learning needs analysis [35]. The needs of the wider health and social care system, including patients and service users, may be established through regional or national priorities, regulatory bodies, coroner’s reports or government-led inquiries, as well as personal and public involvement groups [56–59].
The learning event should be piloted to ensure that it will meet the ILOs [60].
Simulation participants should receive any necessary information in advance, including any assessment criteria; this helps to promote psychological safety, reduce anxiety and maximise learning effectiveness [55,61].
Standard 7: The simulation modality, fidelity and activity design should be determined by the ILOs.
Simulation can be resource-intensive in terms of time, money, staff and equipment [62], but effective simulation does not need to be expensive [63]. For example, low-fidelity, low-cost simulation may be sufficient to deliver curricular outcomes. The modality, fidelity and approach used in the learning event should be determined by the ILOs [64,65].
Whenever multi-professional activities are planned, they should be co-designed by representatives from the involved professions and staff groups in order to develop authentic and inclusive learning opportunities [cv II, standard (s) 6].
Standard 8: Evaluation and research should be considered during the planning stage.
The evaluation of the event and any research activities should be considered during the planning stage. Evaluation of the learning activity allows an assessment of the participant experience, determines how well the ILOs have been met and provides information for continuous improvement. In addition, research into simulation allows the sharing of experiences, processes, and developments with the wider community and helps to improve the quality and impact of simulation [66].
Standard 9: The individual or team facilitating the activity should have training and experience in facilitation, including establishing psychological safety and debriefing.
The adequate facilitation of an activity, including troubleshooting and managing the flow of the scenarios or learning activities, enables effective learning [67,68].
Multi-professional faculty teams should be encouraged. If a learning event is intended to provide interprofessional education, the faculty should be multi-professional [69].
Diversity improves the learning environment [70,71]. Facilitators should have training in equity, diversity and inclusion relevant to simulation-based learning [cv II].
Faculty briefing should take place before the start of the activity [4]. The psychological safety of faculty and participants is a crucial factor for team working, facilitates learning and is an essential element of simulation practice [72–74].
Standard 10: The activity must be initiated by a briefing or pre-briefing which helps create a safe environment where learning can take place.
Simulation briefing or pre-briefing is crucial for the preparation of learners, to optimize their learning experience and to establish a safe learning environment [2,75]. It should:
– Be transparent regarding whether assessment is occurring.
– Clarify the running order of the event.
– Establish ground rules for the activity and the debriefing, including agreements about confidentiality.
– Allow learners to familiarise themselves with the simulation environment and equipment.
– Warn learners of possible learning experiences which may trigger significant emotional responses, and the steps taken to avoid and mitigate these responses [76].
The briefing should also:
– Seek to lower hierarchy gradients, for example by establishing the fallibility of the faculty [77].
– Create an educational contract (fiction contract) in which participants are asked to agree to participate in the simulation as if it is a real event, for the purposes of learning, and facilitators appreciate the limitations imposed by the simulated nature of the event [2].
– Clarify roles, including the roles of any SP.
Standard 11: The purpose of the activity should be to ensure the achievement of the ILOs.
The activity should be focused on participants and their needs, including the ILOs, but should also address emerging needs that may become apparent during the activity [78,79].
Standard 12: The simulated experience must include facilitated reflection or debriefing, in which the participants should explore and develop strategies to improve individual, team and system performance.
The terms ‘observer’ and ‘facilitator’ describe the persons observing and facilitating simulated practice, these might be faculty or participants themselves. In some simulation modalities, these roles may be performed by software or other technologies; in such cases, these standards are designed to apply to the design of those technologies.
Assessment of performance is an integral aspect of all learning [35]. The methods of assessment should match the purpose of the activity, for instance, formative assessment by a skilled facilitator making notes, or summative assessment by a skilled observer using a checklist [55].
If SP take part in the debriefing process, they should be supported and appropriately trained for their role in debriefing [52].
The facilitated reflection, which might include feedback, debriefing or coaching, should be focused on the ILOs, and should follow a structure [74]. Opportunities should be provided to explore the mental frames of the participants [80].
The exploration and development of strategies for improvement must include a process where serious performance-related safety concerns are addressed [36,55].
A participant’s performance in a simulated experience that does not meet an expected standard may be due to many factors outside the participant’s control, from scenario design to simulator malfunction to scenario direction. By definition, the simulated event is not real; faculty should avoid framing performance in the simulated event as a marker of performance in everyday practice.
Poor performance may also reflect burnout or fatigue, rather than a lack of knowledge or skill [81]. However, problematic and unprofessional behaviours that are not event-specific (including such things as racist, abusive, or misogynistic language, drunkenness, etc.) always need to be clearly addressed.
Written protocols must be in place to set out the faculty response to serious concerns regarding unprofessional or abusive behaviour. While many learning events are preceded by a confidentiality agreement (e.g. ‘whatever happens here, stays here’), this may need to be broken, with careful judgement and in exceptional circumstances, to protect the learner or others.
Standard 13: The use of simulation for summative assessments should prioritize validity, reliability and psychological safety.
Where simulation activity is used as summative assessment, assessors should have training in the assessment tool and in the mitigation of conscious and unconscious bias, and should undertake a standardisation process to improve reliability [82]. Tools used in summative and ‘high stakes’ assessments should be valid and reliable [83].
Psychological safety of the learner must be considered, and appropriately supported. To maximize the potential learning, opportunities for feedback, such as a structured debriefing, should follow any summative assessment.
Standard 14: The activity should be evaluated by participants and faculty to inform future activities and, where applicable, system improvement.
Evaluation is an essential part of quality assurance and improvement for simulation activity [84,85].
A thorough evaluation should include:
– feedback on the facilitator’s debriefing skills, and on the SP’s skills in portraying their role.
– a review of the event using an equity, diversity and inclusion (EDI) lens [86].
– mapping to Kirkpatrick or translational science levels and exploring the most important or meaningful outcomes [87].
– documentation of any latent errors or system failures that may have been identified during simulated activity or debriefing, as well as the process that needs to be followed to address them.
The faculty should keep a record of any iterative changes made to the simulation activity in response to evaluation feedback.
Standard 15: Simulation-related research should be of high quality and carried out ethically.
Research is crucial for the advancement of simulation practice, benefiting patients, communities, staff and the systems within which they work. Simulation-related research may be used to advance simulation practice itself, or to explore other questions in wider health and care contexts [33,88]. It should address gaps within existing evidence and help meet the needs of the wider health and care community [89].
It must be carried out within local and national governance structures, including ethical approval processes where appropriate.
High-quality research on simulation activity should be prioritised during the planning stage [s 8], and appropriately resourced in terms of time, funding and personnel. The safety of learners, patients and others must be preserved during any research activity, including after refusal to participate in the research [90,91].
Research should be planned and reported using recognized methodological frameworks, with consideration given to prior work and to the potential impact that could be generated [92].
Where possible, research should be a collaborative endeavour, with diverse contributors in terms of expertise, experience, professional background and location. In the interest of advancing the field of study, negative results and findings should be shared with the simulation community, so as to reduce repetition of unnecessary research [93].
Simulated practice involves interaction between people, resources and the environment. The framework for resource management should include developing a learning environment and culture, promoting educational governance, developing and encouraging learners and leaders, and developing a sustainable workforce [94].
Resource management includes management of simulation, human, financial and digital resources, which requires policies, strategy and leadership. Organizational objectives, inclusive leadership and provision of an equitable learning environment should guide the use of resources.
Standard 16: There should be a clear vision, mission and strategy to sustain and grow simulation practice in alignment with wider organizational and stakeholders’ needs.
The strategy should effectively integrate various aspects of the programme and its goals, including needs assessment, short- and long-term strategies, identification of leadership and management roles, and involvement of stakeholders [95]. It should address how simulation is supported across the organization, including integrating the organizational culture of life-long learning, mentoring and reflective practice. The strategy should also guide faculty development, programme creation and regular review of activities [96].
There should be a dynamic, adaptive collaboration among all stakeholders, including leaders, simulation practitioners, patients, service users, educators and learners [95,96].
Simulation activities should act as a quality and risk management resource for organizations to achieve the goals of improved patient safety and quality [96–98]. Translational and transformative simulation have important roles to play in quality improvement, as they can be used to identify both good practice and latent errors in clinical environments, and should be actively promoted [32,33].
Simulation practice is often under-resourced. Appropriate management and administrative staff should be available and adequately trained to support simulation practice. Faculty development initiatives and fellowship programmes should serve to ensure the delivery of simulation activities [96].
A business plan should identify funding for appropriate space, equipment, resources and the expertise necessary to operate sustainably, and to meet outcomes for all facets of the programme [95]. Financial planning should identify appropriate capital expenditures, address return on investment and identify an appropriate review cycle [50,95,96]. There should be a plan for securing and managing financial resources to support stability, sustainability and growth of the simulation goals and outcomes [cv III].
Standard 17: Designated leads with organizational influence, appropriate expertise and accountability should oversee the design and delivery of simulation activities and use of resources.
The designated leads should:
– have organizational influence, with appropriate oversight by and representation on relevant governance structures.
– have appropriate expertise, detailed in a job description or role specification.
– provide opportunity for growth of leadership skills [96].
– have plans for sustaining simulation activity.
– advocate for the broad application of simulation.
– involve key stakeholders in facility management and governance [95].
– ensure adequate emphasis is placed on recruitment, development and retention of simulation faculty [48].
Standard 18: Robust policies should be in place to ensure prioritization, financial support, quality assurance and safety.
Organizational policies should address:
– clear prioritization of activities and use of resources to ensure best use of space, time, workforce and equipment.
– confidentiality and safe sharing of information and data.
– periodic (at least annual) reviews of simulation-based activities and quality assurance.
– periodic (at least annual) financial review, which also considers return on investment, necessary capital expenditure, growth and sustainability.
– health and safety, including the safe storage and maintenance of equipment and supplies, especially highlighting the need to separate simulation and patient care records and other resources [50,98], including drugs and equipment [95–97,99].
– clear processes for risk assessment and risk registration, within an overall patient safety context [100,101].
– receiving and responding to complaints [94].
All policies should be inclusive, promote equitable learning environments [55,94] and encourage self-reflection [96].
Appropriate recognition of faculty should be provided to maximise retention, and mentoring structures for novice simulation faculty should be in place [50,95,96].
We wish to thank all contributors during the different development phases:
Initial consultation:
– Attendees to online sessions on 22nd September, 26th September and 3rd October 2022, from England, Wales, Scotland, Ireland, India and Singapore: D Baxter, D Byrne, C Burlacu, S Cook, I Curran, J Davies, D De, P Gurnett, C Hawker, S Jone, S Kersey, S Mitra, K Olson, S Orugant, B Pittaway, A Platt, B Reid-McDermott M Sandhukan, E Sreekumar, K Sterling, R Stubbs, D Suggit, R Stiger, A Wilford, J Wright, M Wright.
– Attendees to the workshop held during the ASPiH Annual Meeting on 17th October 2022.
Peer reviewers: S Armijo, Chile; B Baxendale, England; C Burlacu, Ireland; A Buttery, England; SC Cook, Wales; S Edgar, Scotland; E Leon, Spain; R Makker, England; D Nestel, Australia; N Oliver, Australia; N Shiner, England; C Sa Couto, Portugal; M Morrow, Northern Ireland; S Qvindesland, Norway; G Reedy, England; A Romanos, Spain; J Roome, England; P O’Connor, Ireland; A Platt, England; R Szabo Australia.
Institutions contributing to the second round of consultation following peer review: Academy of Medical Educators, UK; Body Interact, Portugal; Cardiff and Vale University Health Board, UK; Faculty of Intensive Care Medicine, UK; Guys and St Thomas’ NHS Foundation Trust, UK Health Education and Improvement Wales, UK; Homerton Healthcare NHS Foundation Trust, UK Karel de Grote University College, Belgium; London Simulation Regional Network, UK; Maudsley Learning, South London and Maudsley, UK; NHS Education for Scotland (NES), UK; North East Simulation Network, UK; Northern Ireland Medical & Dental Training Agency, UK; Nursing and Midwifery Council, UK; Oxford Brookes University, UK; Queen’s University Belfast, UK; Royal College of Anaesthetists, UK; Royal College of Nursing, UK; Royal College of Ophthalmologists, UK; Royal College of Pathologists, UK; Royal College of Physicians, Edinburgh, UK; Royal College of Physicians, London, UK; Royal College of Physicians of Ireland, Ireland; Royal College of Physicians and Surgeons, Glasgow, UK; Royal College of Radiologists, UK; Royal College of Surgeons of Ireland, Ireland; Sociedad Argentina de Simulación (SASIM), Argentina; Sociedad Española de Simulación Clínica y Seguridad del Paciente (SESSEP), Spain; Sociedade Portuguesa de Simulação Aplicada às Ciências da Saúde (SPSim), Portugal; Society for Simulation in Europe (SESAM), Germany; Society for Simulation in Healthcare (SSIH), USA; South Puget Sound Community College, Washington, USA; SimComm Academy, UK; Simulation and Immersive Learning Technologies Programme NHS England, UK; Simulation Based Education, Technology Enhanced Learning and Patient Safety, South East NHS England, UK; Swansea University, UK; The Irish Centre for Applied Patient Safety and Simulation, Galway, Ireland; The Chartered Society of Physiotherapy, UK University Hospitals of Derby and Burton, UK; University of Alabama at Birmingham, USA; University of Greenwich, UK; University of Hertfordshire, UK; University of Portsmouth, UK; West Midlands simulation Network, NHSE Midlands, UK.
Authors’ contributions
None declared.
None declared.
None declared.
None declared.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
83.
84.
85.
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.