
Medical students and residents at our institution perceived a lack of intervention by faculty when incidents of microaggression or bias occur. Although learners receive training on the topic, they often lack the authority to address such issues during clinical rotations. We also recognized that faculty lacked the tools to address bias and microaggressions, hindering meaningful discussions. The absence of dialogue perpetuates bias and microaggressions, adversely impacting under-represented groups and minorities. While practising dialogue has increased confidence during uncomfortable encounters amongst trainees [1,2], its application among faculty remains limited.
Traditional education initiatives emphasize conceptual understanding of bias and microaggressions. While such passive training has been criticized for its limited impact on changing institutional culture [3], interactive activities have proved promising [4]. Thus, we designed and evaluated an experiential course for faculty, aiming to deepen their understanding of bias/microaggression and equip them with tools to lead meaningful dialogue.
Even in situations less charged than those involving bias and microaggressions, clinicians often find it challenging to provide feedback. In response, Rudolph et al. [5] developed the PAAIL (Preview–Advocacy1–Advocacy2 –Inquiry–Listen) framework to facilitate meaningful debriefing in a range of situations. We adapted this framework and added the Bridge-the-Gap component to support conversations around bias and microaggressions in healthcare education (Figure 1).

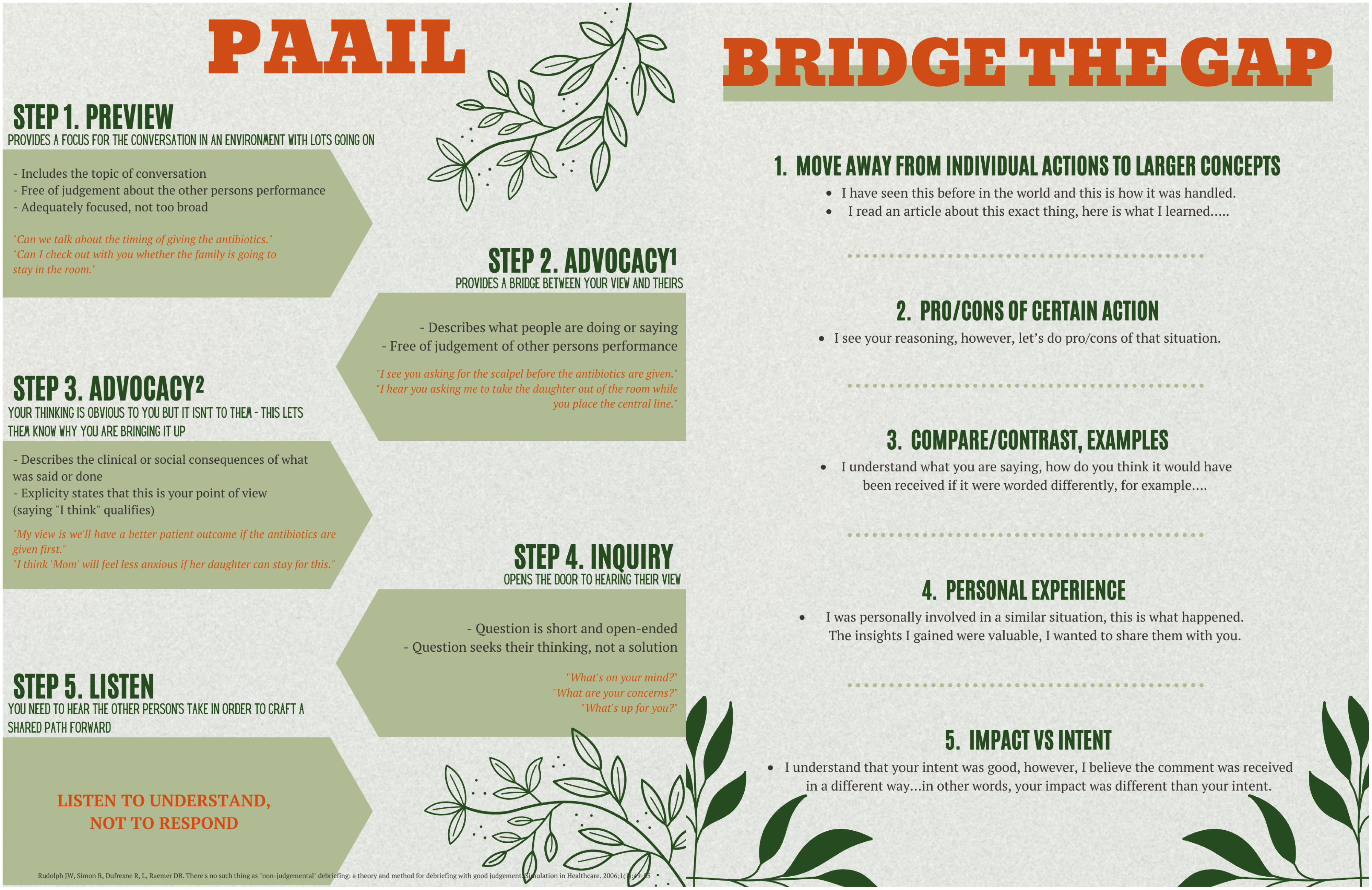
PAAIL and Bridge-the-Gap framework for bystander intervention.
Our demographically diverse team created a course to (1) familiarize participants with foundational concepts, (2) introduce and practise the PAAIL+B framework for bystander intervention, and (3) evaluate the programme’s impact via a survey 6-week post-simulation activity. Medical faculty volunteers who provided consent participated in this IRB-approved study. The 3-month course was taught by three of its developers to 15 participants. It consisted of four 2-hour sessions: the first three were conducted on Zoom and the fourth was held in-person. The Zoom sessions consisted of pre-briefing, review of definitions and introduction to the PAAIL+B methodology. Instructors discussed resources available for faculty experiencing overt racism and sexism, factors to consider before speaking up, and implications of choosing between ‘calling in’ and ‘calling out’ in the workplace. Participants practiced the PAAIL+B approach in breakout groups that were facilitated by the instructors.
During the in-person session, participants engaged with trained simulated participants (SPs) in various staged microaggression encounters based on officially reported incidents (Table 1). After receiving an orientation and preparing their dialogue strategy, faculty participants entered their ‘office’ where their colleague ‘aggressor’ was waiting to discuss the reported incident. The encounters varied in severity of microaggression, authority gradients and incident setting. SPs were trained to adjust their pushback based on the learner’s evident comfort. Each encounter concluded with a debriefing.

| SP case overview | Setting | |
|---|---|---|
| Case 1 | Dr. Sulley is a second-year resident in the university-sponsored radiation oncology programme. She graduated from Harvard Medical School. She did very well as a first-year resident, scoring second highest on the in-training exam for her class, and has had two publications accepted on her work on improving quality of life of patients receiving radiation. During her rotation on the breast oncology service, one of the faculty members, Dr. Adler, asked her about her interest in radiation oncology in the following manner: ‘It is an interesting specialty choice for a woman. All the physics and math, why would a pretty woman like you be interested in that? I mean, where’s the glamour?’ She politely replied: ‘I love math and physics. I was a math major at Harvard, and I thought that radiation oncology would be perfect for me. And my looks have nothing to do with it.’ The next day at conference, after a clinical question was asked, Dr. Adler called out: ‘Where’s Miss Math Genius?’ pointing at Dr. Sulley. ‘I am sure she knows the answer’. She went on to answer correctly. Later that day, in a hallway encounter, Dr. Adler said: ‘Good work, Smarty Pants, let’s see what you can do next time’. She encountered him 2 weeks later in the clinic. He called out as she approached, ‘Here comes the beautiful Miss Math Genius’. The group around him laughed. Embarrassed, Dr. Sulley left the clinical area and waited an hour to see the patient. |
Your office. You are the programme director. You have asked Dr. Adler for time to speak about a recent resident interaction. He was annoyed but agreed. You have known him for 15 years and he tends to be a bit of a curmudgeon but the two of you have always maintained a working relationship. He gets himself into trouble from time to time, and although he does not always accept feedback well, he does make course direction changes eventually. Dr. Sulley will not be present at this meeting. Dr. Adler is waiting for you in your office. |
| Case 2 | [Bystander] You are standing with a group of colleagues in the preoperative area, a [new nurse, Marcelle] in the PACU introduces herself to the group. A new [junior colleague/attending] Dr. Green says, ‘What are you? You’re so interesting looking’. A few people in the group look visibly uncomfortable. The new nurse, Marcelle, looks mortified and uncomfortable. She sighs and then gracefully answers that she is from New Jersey, but her mother is Haitian, and her father is from Trinidad. You [Bystander] like the junior attending, Dr. Green, and although it’s not your role, you feel the need as a senior faculty member in your department to inquire and start dialogue with him. |
You notice that Dr. Green is in his office, and you ask if you can speak about the interaction that happened yesterday in PACU. The nurse is not present at this meeting. |
| Case 3 | You [bystander] are serving on a 12-person selection committee for a new chair of a department. At the first meeting, during a lengthy discussion of several diverse candidates, a few selection committee members point out the accomplishments of Dr. Suarez and Dr. Munagala with respect to their historically marginalized identities and systematic racism and bias that they face. One committee member even suggested changing the rating rubric to account for these struggles since most people who hold marginalized identities have faced systemic discrimination in the past. These people do not have the same opportunities to attend an ivy league school, for example. Three candidates have similar credentials but from diverse backgrounds: 1. Thomas Peterson: Ivy league Pedigree, now Vice Chair at Department of top medical school, 100 papers 2. Alyssa Suarez: First generation physician, attended highly ranked medical school, now Vice Chair in a second tier (but solid) Department in a smaller health system. 100 papers 3. Anish Munagala: First generation American, attended lesser-known medical school, Chair of a small Department for 10 years in a small town. 150 papers. A [senior white male faculty member – Dr. Jacobs] that is your acquaintance says, ‘This is simple, I believe the most qualified person should get the job. I know Tom’s father- they are a good family and I have known Tom for more than 20 years, he even worked in my lab when he was first starting out- besides, he has the pedigree. Since a number of us also attended the same school as Dr. Peterson, we know what we are getting’. A few people agree with this statement, but it didn’t sit right with you. You could not pinpoint why you were feeling this way at the moment and decided to let it go. You sleep on it, and you are still bothered the next day. You email him and ask him for 10 minutes to touch base regarding the last selection committee meeting. |
You’ve emailed Dr. Jacobs asking him to meet after a statement he made at the selection committee meeting regarding a candidate that is still bothering you after you slept on it. He is your acquaintance. You are now outside his office ready to knock on the door for the meeting. |
Participants completed a pre-course Qualtrics survey created by the authors to measure baseline knowledge and attitudes. During the initial virtual session, qualitative feedback from participants was collected. SPs and observers provided formative feedback to participants using an internally developed three-point rating scale based on the PAAIL+B method. Next, we collected feedback from participants during the debriefing to target course improvement. A 6-week follow-up session intended to assess the course impact was cancelled because of participant unavailability.
The 15 self-selected participants indicated that they had all personally experienced or witnessed bias and microaggressions first hand. From the pre-course survey, most participants rated themselves as either moderately or very familiar (75%) with the term microaggression. Only 25% self-rated as slightly or extremely familiar with the term. In terms of recognizing microaggressions, 75% felt moderately to very confident, while 25% felt slightly confident.
Initial resistance and scepticism about the study’s institutional motives were evident. Some participants preferred not having others advocate for them to avoid potential repercussions when dealing with aggressors. Others were uncomfortable engaging discussion with real-life ‘aggressors’. Factors such as gauging one’s emotional capacity, evaluating safety and deciding when to converse with the aggressor were also highlighted.
Regarding the execution of the PAAIL+B steps, 47% of participant ratings were ‘developing’ and 47% were ‘proficient’.
Although the focus of this course was on the steps to follow immediately after witnessing bias or microaggressions in general, it became clear that emphasizing validation of these experiences within the local institutional culture would increase its impact. This was particularly evident considering the unresolved trauma many participants carry from prior workplace incidents.
While the initial aim was to empower faculty with effective dialogue tools, we realized that fostering a deeper institutional understanding of bias and microaggressions is essential for genuinely impactful conversations on these sensitive topics.
The course offered clinical faculty a framework to intervene in cases of bias and microaggressions. Next, we aim to evaluate whether practising challenging conversations increases psychological safety and confidence among faculty during such discussions. Specifically, we seek to determine whether heightened safety and confidence promote more frequent faculty-led dialogues on these topics. Ultimately, our goal is to ascertain if normalizing these conversations fosters inclusivity and engagement among faculty, staff and learners.
Vikasni Mohan: Writing - original draft, writing - review and editing; Samantha Syms: Conceptualization, methodology, data curation, writing - original draft, writing - review and editing; Ilya Shekhter: Conceptualization, methodology; Miriam Lipsky: Conceptualization, methodology; Nanette Vega: Conceptualization, methodology; Danielle Bodzin Horn: Writing - original draft, writing - review and editing; Barry Issenberg: Writing - review and editing; Joni Maga: Conceptualization, methodology, writing - original draft, writing - review and editing.
None declared.
None declared.
None declared.
None declared.
1.
2.
3.
4.
5.