Creating additional placements for undergraduate paramedic learners is being driven by Health Education England (HEE). With the increase in numbers undertaking paramedic training by education providers, there is limited additional capacity for placements within the current placement areas (e.g. Ambulance Trusts).
Working in partnership with a dedicated simulation team, the paramedic science lecturers co-created a simulated placement. One aspect included the students undertaking a one-day ‘Train the trainer course’ prior to the day of facilitating led by the simulation lecturer and this course referred to research and best practice standards [1]. Seventy-six third-year students across two different cohorts undertook this activity. From two cohorts, eleven different simulation activities were created. Three focused on trauma injuries (e.g., a severed arm in a factory). In the remaining eight simulation designs, the paramedic students chose areas of their professional practice they wanted to focus on, including a lady with domestic violence.
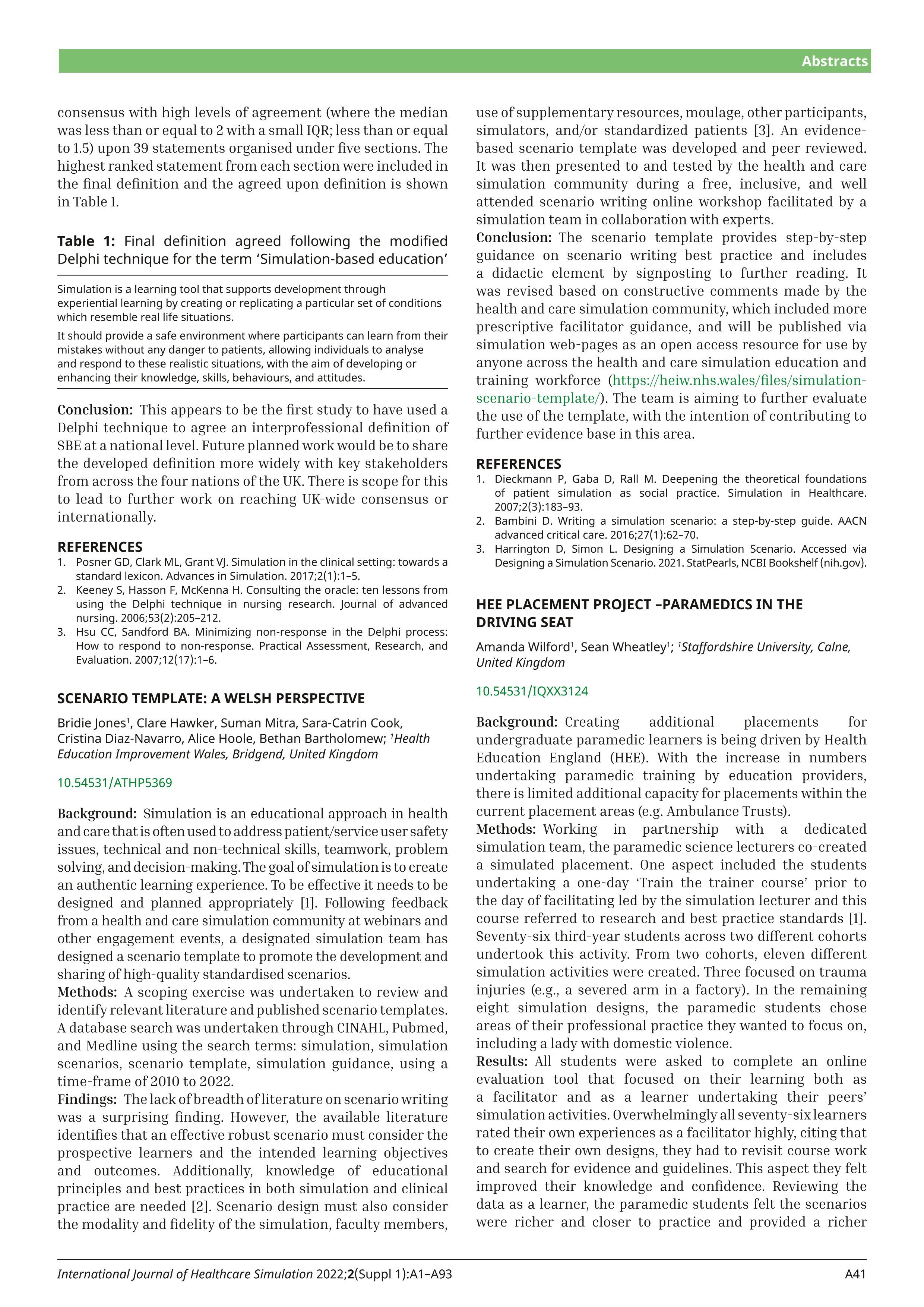
All students were asked to complete an online evaluation tool that focused on their learning both as a facilitator and as a learner undertaking their peers’ simulation activities. Overwhelmingly all seventy-six learners rated their own experiences as a facilitator highly, citing that to create their own designs, they had to revisit course work and search for evidence and guidelines. This aspect they felt improved their knowledge and confidence. Reviewing the data as a learner, the paramedic students felt the scenarios were richer and closer to practice and provided a richer discussion. Participating in debriefing as both the facilitator and learner, the participants reported that they felt more comfortable about critiquing care that learning how to use open questions.
The students created their own community of practice [2] and actively sought literature and evidence-based practice to create the designs and the parameters and behaviours for their own cases that they facilitated. The debriefing sessions evolved into reflection surrounding their identity and the agency of practice in the clinical arena. As faculty, the expectations prior to this project were that the designs created would be trauma only and found all were authentic and professionally written. The faculty will be implementing this project across all years of undergraduate training for paramedics. Supporting students to write and deliver their own SBES at intervals allows them to be involved in their own learning. This additional knowledge and skills will assist them into professional practice.
1. Persico L, Belle A, DiGregorio H, Wilson-Keates B, Shelton C. Healthcare simulation standards of best practiceTM facilitation. Clinical Simulation in Nursing. 2021;58:22–26.
2. Wenger E. Communities of practice: learning, meaning, and identity. 1999. Cambridge, UK, Cambridge University Press.