
Since the origins of surgery, simulation has played an important role in surgical education, particularly in plastic and reconstructive surgery. This has greater relevance in contemporary settings of reduced clinical exposure resulting in limited work-based learning opportunities. With changing surgical curricula, it is prescient to examine the role of simulation in plastic and reconstructive surgery.
A scoping review protocol was used to identify relevant studies, with an iterative process identifying, reviewing and charting the data to derive reported outcomes and themes.
Of the 554 studies identified, 52 studies were included in this review. The themes identified included simulator modalities, curriculum elements targeted and relevant surgical competencies. There was a predominance of synthetically based simulators, targeting technical skills largely associated with microsurgery, paediatric surgery and craniomaxillofacial surgery.
Existing simulators largely address high-complexity procedures. There are multiple under-represented areas, including low-complexity procedures and simulation activities addressing communication, collaboration, management and leadership. There are many opportunities for simulation in surgical education, which requires a contextual appreciation of educational theory. Simulation may be used both as a learning method and as an assessment tool.
This review describes the literature relating to simulation in plastic and reconstructive surgery and proposes opportunities for incorporating simulation in a broader sense, in the surgical curriculum.
The growing expectations of proficiency and service delivery, combined with diminished surgical exposure due to restricted working hours and fewer opportunities for clinical teaching, result in reduced opportunities for work-based learning [1]. Despite the move to competency-based training, surgical education and training time remain largely fixed. The COVID-19 pandemic has compromised conventional training opportunities [2]. While already embedded in many training programmes, a simulation may become an essential solution for supporting the acquisition of new techniques, for assessing competence and for maintenance of skills [3].
Plastic and reconstructive surgery is the oldest documented surgical specialty, tracing its origins to Susruta’s description of nasal reconstruction [4]. Simulation of surgical procedures with models dates back to this time [5] revealing simulation as one of the oldest educational methods and with demonstrated relevance to plastic surgery. However, the use of simulation has arguably increased with the rapid pace of surgical developments seen in contemporary practice. Kazan et al [6] provide a graphical representation of some simulator advancements in plastic surgery. Technology has increased the realism and complexity offered by simulators.
Simulation enables the learner to participate in experiential activities with varying degrees of realism and affording opportunities for reflection, feedback and debriefing [1]. Furthermore, there is the potential to achieve mastery via repetitive and deliberate practice [7], with no risk to patients. Simulation seems an ideal tool for contemporary surgical education.
Encompassing such a broad range of subspecialties, plastic surgery has the opportunity for many simulation modalities to support trainees’ learning. Indeed, this field has been the subject of a number of studies, including recent reviews on simulation in reconstructive and aesthetic surgery [8]. Curricula are often structured according to themed competencies that cumulatively reflect holistic practice [9]. Accordingly, it is necessary to evaluate the incorporation of simulation in this holistic context. With the recognition of the role of the surgeon beyond that of a technician, the place of simulation in surgical education warrants exploration. To this end, we performed a scoping review to assess the current use of simulation identifying future opportunities for simulation in plastic and reconstructive surgery education and training.
As described in a previous article (2), the methodological framework articulated by Arksey and O′Malley was used as the basis for our scoping review, adhering to five phases: (1) identifying the research question; (2) identifying relevant studies; (3) study selection; (4) charting the data; and (5) collating, summarizing and reporting the results [10].
In this review, we sought to identify simulation modalities used in plastic and reconstructive surgical training, with particular reference to both plastic and reconstructive surgery competencies and essential surgical competencies. Accordingly, the research question posed was ‘what types of simulation modalities are used in plastic and reconstructive surgery training?’. A further sub-question was ‘how does simulation-based training address achievement of both plastic and reconstructive surgery-specific competencies and essential surgical competencies?’
In accordance with the Population, Context, Concept (PCC) framework [11], a protocol investigating simulation in education and training for plastic and reconstructive surgery was developed (Table 1). The search targeted plastic and reconstructive surgery trainees. The concept was simulation and simulation modalities. The context included competencies, related specifically to plastic and reconstructive surgery and to essential competencies.

| Population terminology | Plastic |
|---|---|
| Concept terminology | Simulat*, education, training, learning |
| Context terminology | Plastic, reconstructive, skin, soft tissue, aesthetic, esthetic, cosmetic, burn, craniofacial, craniomaxillofacial, head and neck, hand, breast, chest, trunk, perineum, lower limb, paediatric plastic, pediatric plastic, microsurgery, competenc*, communication, teamwork, collaboration, management, leadership, health advocacy, scholarship, teaching, professionalism, ethics |
| Search strategy | (Simulation Training/ or simulat*) AND (plastic) AND (education or training or learning) AND ((plastic or reconstructive or skin or soft tissue or aesthetic or esthetic or cosmetic or burn or craniofacial or craniomaxillofacial or (head and neck) or hand or breast or chest or trunk or perineum or lower limb or paediatric plastic or pediatric plastic or microsurgery) OR (competenc* or communication or teamwork or collaboration or management or leadership or health advocacy or scholarship or teaching or professionalism or ethics)) |
| Medical subject heading terms | Simulation Training/ |
A search strategy was developed with the intention of capturing maximal results initially, subject to subsequent refinement. Search terms included ‘simulation’ with truncation to maximize search results, ‘plastic’, ‘education’, ‘training’ and ‘learning’. Further terms were added from Curriculum 2019, the most recent revision of the Plastic and Reconstructive Surgery Curriculum, which defines both Plastic and Reconstructive Surgery Competencies and Essential Surgical Competencies [12].
The first author (MAS) conducted the search on 28 May 2021, initially identifying sources in three Ovid MEDLINE databases (MEDLINE, In-Process & Other Non-Indexed Citations and Epub Ahead of Print). A subsequent search of the ERIC (Education Resources Information Centre) database was conducted with an identical search strategy. English language was used as a filter at the conclusion of the search. There were no qualifications on date or publication type employed. A search of the grey literature was not conducted given the volume of sources identified from existing databases.
As a result of the extensive breadth of subject matter and constraints on our resources, exclusion criteria were determined. The iterative nature of this process ensured that these criteria were modified in the development of a sound search strategy. A requirement of only English-language literature circumvented the need for translation of material which would have proved both time and resource consuming. Additional exclusion criteria were imposed throughout the process (Table 2).

| Exclusion criteria | Non-English language source |
|---|---|
| Sources discussing simulator development without reference to educational impact | |
| Sources discussing courses incorporating simulation but without specific discussion of the simulators | |
| Sources discussing the use of simulation without reference to education | |
| Sources discussing simulation in education of undergraduate medical students | |
| Sources relating to specialties other than plastic and reconstructive surgery | |
| Duplicate source |
Titles were screened independently by two authors (MAS and ABY). Sources proceeded to abstract review where authors agreed on inclusion or where there was disagreement. A predetermined strategy for addressing disagreement involved an independent review of source inclusion by each author. If disagreement remained, referral to a third author (DN) was used to resolve disagreement. Sources where authors agreed that titles be excluded led to exclusion. A similar process was undertaken in the abstract review phase. Additionally, any source without an abstract automatically progressed to full-text review where the same consultative process was repeated.
The data charting phase involved the synthesis and interpretation of data by sorting the material thematically [10]. Variables aligned with the PCC components of the research question were defined and inserted into a data charting form using Microsoft Excel (Microsoft Excel for Mac, 2020, Microsoft Corporation, Redmond, Washington). Demographics of the publications were included in the charting form. Further variables were added to the spreadsheet during the charting phase in response to the iterative nature of charting. Two authors (MAS and ABY) extracted the data, and a consultative process was undertaken to ensure the accuracy of charting. Disagreements were resolved by either consensus or failing that referral to a third author (DN).
The final stage of the scoping review framework relates to the presentation and analysis of the results as outlined below.
The initial database searches yielded 554 sources, which was reduced to 538 when results were limited to English-language sources. Title and abstract screens resulted in the exclusion of 391 and 46 results, respectively, following which a full-text review occurred. Further restriction of sources proceeded according to exclusion criteria determined via the iterative process inherent in a scoping review. One paper was excluded as it was reporting the evaluation of a simulator already included in the search results, and another was identified as a duplicate despite a reversal of author order. Thus, 52 sources were included in the scoping review (Figure 1) (Appendix A).

![PRISMA flow diagram (adapted from Moher et al [13]) of the literature search (conducted on 28 May 2021) and study selection process for this scoping review on simulation in plastic and reconstructive surgery.](/dataresources/articles/contents-1656068944654-3c4afcc0-fb10-45ee-b5ad-53e1bf1ac960/assets/ijaa019f0001.jpg)
PRISMA flow diagram (adapted from Moher et al [13]) of the literature search (conducted on 28 May 2021) and study selection process for this scoping review on simulation in plastic and reconstructive surgery.
The characteristics of included studies are presented in Table 3. The majority of sources originated from North America (28, 53.8%), predominantly the USA (22, 42.3%). Fourteen (26.9%) were from Europe, mainly the United Kingdom (8, 15.3%), with the remaining 19.3% of sources from Asia (8, 15.5%) and South America (2, 3.8%). While results were identified from 26 journals, 48 sources (92.3) were published in surgical journals; out of those, 14 (26.9%) sources were published in Plastic and Reconstructive Surgery (Lippincott, Williams & Wilkins), in either subscription or open access formats. The remaining four (7.7%) were published in either education or medical journals. One source [14] provided a guide for building a microsurgery simulation course and included multiple simulators and was classified as a review for the purposes of this study. Eleven review articles (21.1%) were included.

| Year | ≤2000 [15,16] | 2001–2005 [17,18] | 2006–2010 [19] | 2011–2015 [20–28] | 2016–2020 [6,14,29–59] | 2021 [8,60–63] |
| Number of authors | 1–2 [23,26,51,60] | 3–4 [15–20,24, 25,27, 28,31,34,35, 39,41,45,49,59] | 5–6 [6,14,22,29,32,36,37, 40,44, 48,50,52,53,55–58,62] | 7–8 [21,30,33,38,42,46,47,54, 61,63] | 9–10 [8,43] | |
| Continent of origin | North America [6,17,19–23,25–31,33,34,36, 42–45,51–53,55,56 ,58,63] | Europe [14,16,18,32, 37,39,41,48–50, 54,60–62] | Asia [15,24,35,38,40,46,47,57] | South America [8,59] | ||
| Publication type | Surgical [6,8,15–27,29–52, 54–57,59–63] | Education [14,53] | Medical [28,58] | |||
| Article type | Original article [15,17,19–26, 32–41,43–46, 48–50,52,54,56–59,61–63] | Review article [6,8,14,27–30,42,47,55,60] | Letter to editor/ editor’s choice [16,18,31,51] | Innovation/ technical/ experimental section [53] |
Despite some overlap with either simulator material or targeted skill-set, 42 different simulators were reported in individual articles. Further modalities were reported in the review articles (each considered a single source in this review). The most widely reported form of simulator was a prosthetic/synthetic simulator (30, 55.6%), followed by cadaveric models – human (15, 27.8%) and animal (13, 24.1%). Three sources (5.6%) described the use of fruit for skin graft harvesting [ 31,35] and dermatologic procedures [28] (Figure 2).

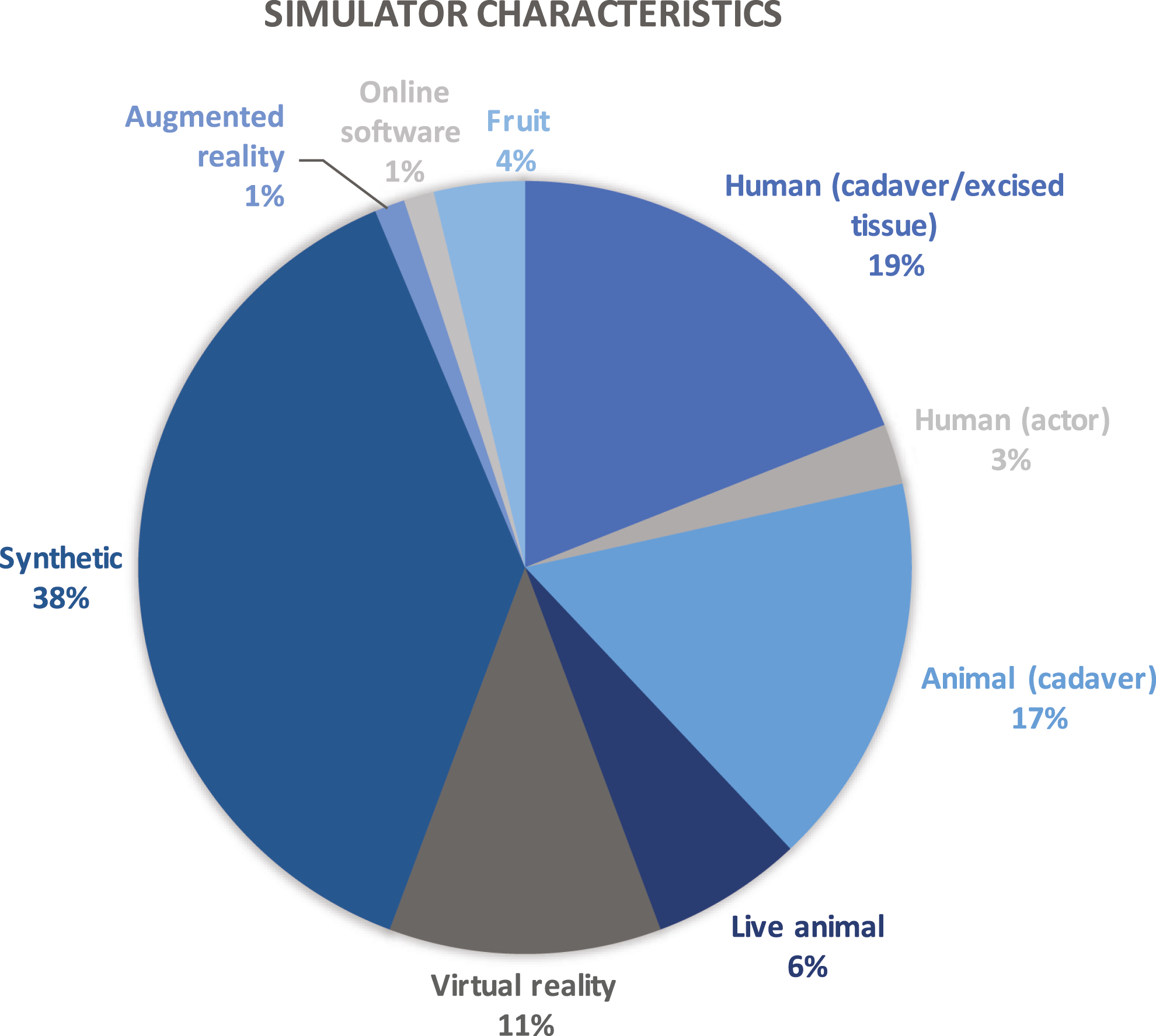
Simulator characteristics identified in included sources, represented graphically.
When considering the curriculum areas of the plastic and reconstructive surgery curriculum [12], there was a wide range of topics (Figure 3). The majority of simulators addressed microsurgery (19, 35.2%), whereas 16 (29.6%) were related to skin and soft-tissue procedures, followed by craniomaxillofacial (14, 25.9%), paediatric (11, 20.4%) and hand surgery (11, 20.4%). Notably, where there were simulators addressing multiple curriculum areas, such as paediatric craniomaxillofacial procedures, the simulators were included under both areas (e.g. cleft palate simulators are classified as both craniomaxillofacial and paediatric).

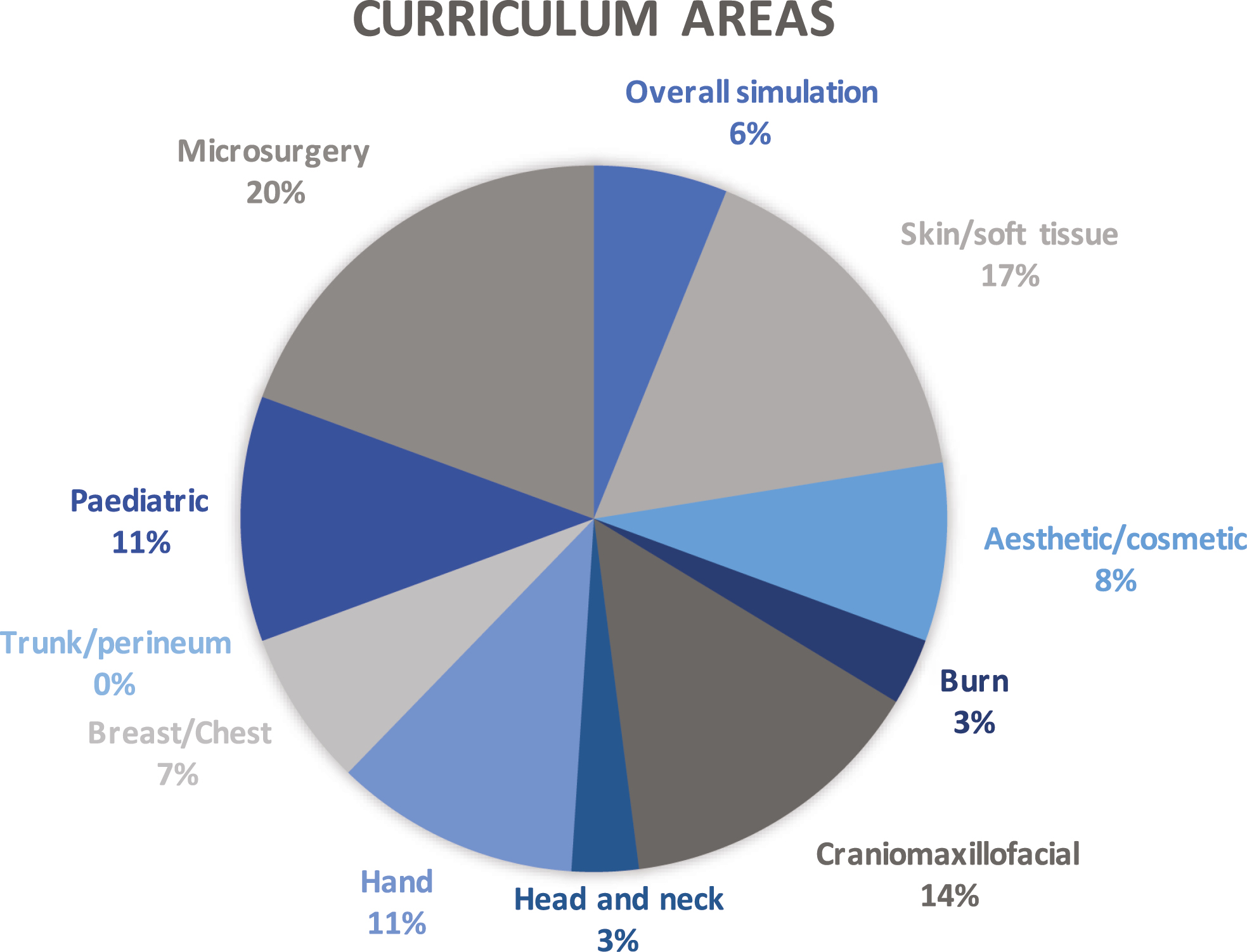
Curriculum areas addressed by sources included in this scoping review, represented graphically.
The surgical competencies, as defined by the Royal Australasian College of Surgeons (RACS) [9], encompass the attributes of a practising surgeon. These competencies provide a thematic framework for the analysis of the sources regarding simulation, particularly in identifying the competencies addressed with greater or lesser emphasis by existing simulation (Figure 4). Seven of the sources addressed the competencies in general terms (13.0%). The predominant competency targeted was technical expertise (45, 83.3%). Other competencies for which simulators were used included medical expertise (17, 31.5%) and judgment/clinical decision-making (15, 27.8%). Only three sources addressed communication (5.6%) and a single source used simulation related to professionalism/ethics (1.9%). Of note, there were no sources that used simulators or simulation to address competencies of collaboration/teamwork, management/leadership, health advocacy, cultural competence and safety and scholarship/teaching.

![Royal Australasian College of Surgeons competencies [9] identified in sources included in this review, represented graphically with accompanying table.](/dataresources/articles/contents-1656068944654-3c4afcc0-fb10-45ee-b5ad-53e1bf1ac960/assets/ijaa019f0004.jpg)
Royal Australasian College of Surgeons competencies [9] identified in sources included in this review, represented graphically with accompanying table.

| Competency | Number | Percentage |
|---|---|---|
| General | 7 | 13.0 |
| Technical expertise | 45 | 83.3 |
| Medical expertise | 17 | 31.5 |
| Judgement/clinical decision-making | 15 | 27.8 |
| Communication | 3 | 5.6 |
| Collaboration/teamwork | – | – |
| Management/leadership | – | – |
| Health advocacy | – | – |
| Scholarship/teaching | – | – |
| Professionalism/ethics | 1 | 1.9 |
| Cultural competence and cultural safety | – | – |
This review of 52 sources details the presence of simulation in plastic surgical education, providing insight into opportunities for simulation in this context. Below, we describe simulators and their applications, gaps in simulations and identify opportunities.
The simulators, as identified by this review, consist largely of prosthetic or synthetic materials, followed by cadaveric models. The curriculum areas addressed by the literature are heavily weighted towards microsurgery, skin and soft tissue, as well as craniomaxillofacial and paediatric procedures. When viewed in conjunction, these findings paint a picture of simulators largely addressing higher-complexity procedures. This may be an optimal scenario for simulation as an educational modality, wherein the margin of error may be too narrow to allow for ‘practice’ in a live scenario without the accrual of a pre-requisite skill level. In microsurgical procedures, the difference in sub-millimetre accuracy may prove the difference between success and failure. Similarly, the risk of long-term disfigurement of paediatric craniofacial patients possesses significant psychological and social impact for patients and potential medicolegal ramifications for treating surgeons. The proportionally greater presence of simulation in these areas is likely to borne out of the above considerations.
However, simulation need not be limited to these types of high-complexity procedures. There is a benefit to simulation being employed in lower-complexity procedures, to provide feedback and the improvement of practice [64]. In the learner-centric environment of competency-based medical education, the focus has shifted from relatively few high-complexity situations to multiple low-complexity encounters designed to promote professional development [65]. The psychological and educational safety enables learners to focus on development rather than being concerned about progress through the curriculum [66]. Similarly, learners might benefit from simulation of lower-complexity situations, in which the ramifications of underperformance would not lead to significant patient morbidity but practice would improve holistic patient care. Accordingly, collaboration between simulator developers, surgeons and others involved in surgical curriculum design would promote the development of a wider range of simulators to address a wider range of procedures and clinical scenarios.
A simplistic appreciation of simulation restricts its application to the technical aspects of surgery. However, surgeons need to achieve a range of competencies. Accordingly, this review seeks to examine simulation in plastic surgery through the framework of the surgical competencies as detailed by RACS [9]. Perhaps unsurprisingly, there were few studies addressing communication and professionalism/ethics, with no reference to collaboration/teamwork, management/leadership, health advocacy, cultural competence and safety and scholarship/teaching. While this absence might represent a dated appreciation of the qualities of a surgeon, the relative paucity of simulation in these areas may also reflect challenges in the objective assessment of these competencies. To this end, it may be necessary to either include these competencies in the design of existing simulations or develop additional simulations that would specifically target the under-represented competencies. For example, sequential simulations would provide an opportunity to address a range of competencies linked with communication and professionalism. A patient (simulated) with a skin lesion (tattoo) could be seen pre-procedure for assessing the lesion and explaining treatment options. The trainee then moves to a hybrid simulation (simulated patient with a lesion on skin pad) where the lesion is excised and then to post-procedure, discharging the patient. The sequence can continue in a time-compressed manner to explain histology and further treatment to the simulated patient.
Recreating the complexity of holistic surgical practice in simulation can be challenging, and reducing this complexity risks losing key features. Certain competencies including professionalism are difficult to define and, therefore, to demonstrate in isolation. This may explain the focus on competencies that can be simulated with reduced complexity, such as technical expertise. Moreover, for simulation to be productive, allowing for demonstration of trainee progression, as many variables in the simulation scenario must be controlled or reproduced – a feature that lends itself more readily to some activities over the complex interplays of teamwork or collaboration. The difficulties in the design of simulation targeting these competencies might explain their relative paucity in simulations for plastic surgery.
The advantage of this scoping review lies not in its description of deficiencies but rather in the opportunities for simulation to complement existing educational practices. For this to occur, there must be an appreciation of simulation in a broader sense, beyond technical exercises on synthetic devices. Procedural simulation is largely supported by the educational theories on the development of expertise. Mastery learning [67] incorporates deliberate practice [7], wherein deconstruction of procedures, goal setting and repetitive practice with feedback on performance, can promote the development of expertise. It is the educational design, rather than the simulator itself, which has the ability to promote learning [68]. Beyond procedural simulation are scenario-based simulations where holistic surgical practice can be rehearsed. Additional theories including reflective practice [69], complexity theories [70,71] and socio-cultural theories [72] have all been used in scenario-based simulation designs. The possibilities for incorporating simulation into surgical education are essentially boundless, though their application must be targeted to ensure the best use of resources and maximal benefit to the learner.
The incorporation of multiple elements in a simulation, increasing the realism of the simulation scenario and widening the scope to include multiple competencies, holds great potential for plastic and reconstructive surgical education. Examples of such might include clinical situations in which the challenges associated with diversity might allow for practice of cultural competence and cultural safety, or even team-based scenarios wherein collaboration/teamwork, as well as management/leadership are demonstrable. Whilst team-based learning simulation is already widely used to support the development of team-based surgical and interprofessional communication in other specialties [ 73, 74], this is rarely employed in plastic and reconstructive surgical education. In doing so, simulation might provide a more realistic representation of clinical scenarios, priming the learner for the challenges associated with clinical practice.
With the gradual transition from the Halstedian model of time-based apprenticeship to competency-based medical education [6], surgical curricula internationally are undergoing much change. The elements necessary to be deemed competent often include the successful completion of multiple workplace-based assessments to achieve particular milestones, following which the trainee is then deemed competent. Simulation might be used for formative assessment – namely, low-complexity encounters where the outcome sought is feedback provided for learning rather than of learning. The performance of multiple simulation scenarios designed around a particular curricular element would allow for comparison of the simulations to both demonstrate and inform progress.
Simulation might also be used for summative assessment, with structured simulation incorporated into the formal curriculum. The Objective Structured Clinical Examination (OSCE) in undergraduate education is certainly applicable to postgraduate study. The opportunity to present the learner with a simulated patient who can enable the demonstration of medical expertise, communication, professionalism and even cultural competence and cultural safety should be considered. Furthermore, benchtop simulators might be used to demonstrate technical expertise, should a trainee perform below expected standards.
The scoping review reveals the potential of simulation for formative and summative assessment and for procedural and holistic surgical practice.
The iterative nature of this review provides a holistic view of simulation in plastic surgery, allowing for an appreciation of sources free of the constraints imposed by otherwise restrictive predetermined inclusion and exclusion criteria. The limitations of the study largely relate to excluded sources. A strength of the scoping review approach is the inclusion of sources from grey literature. While we sought to adhere to the scoping review method, the large number of sources balanced against our own resources led us to focus only on conventional databases. We acknowledge this limitation in our review. Furthermore, the title screen may have led to some relevant studies having been excluded, which may not have occurred had all studies undergone abstract review. The decision to screen titles and abstracts separately, as well as the exclusion of non-English literature sources, was also pragmatic and considered available resources. Accordingly, a potential limitation was having not employed librarian services to conduct the search, though we did consider the search to be a significant component of the study and thus undertook this process ourselves rather than outsourcing this process. Both grey literature and non-English sources may have added to the findings and are an important area for future research.
Simulation has been used as an educational modality in plastic and reconstructive surgery for millennia. Simulators have focused on the technical expertise of surgery and have been designed, largely, for high-complexity procedures. With the progression towards competency-based medical education, opportunities to use simulation to address a wider range of competencies is an exciting prospect. Examination of the competencies addressed by existing simulation modalities has revealed certain strengths and avenues of opportunity for the greater implementation of simulation in plastic and reconstructive surgery. This review may provide the impetus for the incorporation of simulation into formal curricula, to better complement existing educational strategies.
All authors contributed equally to this study.
There are no sources of funding for this study.
None.
None declared.
None declared.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.

| First author | Citation | Year | Title | Journal |
|---|---|---|---|---|
| Abi-Rafeh, J | [29] | 2019 | Nonbiological microsurgery simulators in plastic surgery training: a systematic review | Plastic and Reconstructive Surgery |
| Ad-El, DD | [15] | 2000 | Digital replantation teaching model in rats | Microsurgery |
| Agrawal, N | [30] | 2020 | The use of simulation in plastic surgery training | Plastic and Reconstructive Surgery – Global Open |
| The_ASSH_ Surgical_ Simulation_ Taskforce | [31] | 2020 | Establishing validity of a comprehensive hand surgical training and educational platform (STEP) | Journal of Hand Surgery |
| Bari, AS | [20] | 2012 | Overcoming the learning curve: a curriculum-based model for teaching zone II flexor tendon repairs | Plastic and Reconstructive Surgery |
| Bielsa, VF | [60] | 2021 | Virtual reality simulation in plastic surgery training. Literature review | Journal of Plastic, Reconstructive and Aesthetic Surgery |
| Carey, JN | [21] | 2014 | Simulation of plastic surgery and microvascular procedures using perfused fresh human cadavers | Journal of Plastic, Reconstructive and Aesthetic Surgery |
| Carr, S | [32] | 2020 | Determining the effect of external stressors and cognitive distraction on microsurgical skills and performance | Frontiers In Surgery |
| Cheng, H | [33] | 2018 | Teaching palatoplasty using a high-fidelity cleft palate simulator | Plastic and Reconstructive Surgery |
| Christophel, JJ | [34] | 2017 | A facial trauma simulation course for evaluation and treatment of facial fractures | JAMA Facial Plastic Surgery |
| Cohen, AA | [35] | 2020 | “POMELO PROJECT” – a simple and low-cost simulator for harvesting skin graft by plastic surgery residents | Burns |
| D′Souza, N | [22] | 2015 | Teaching facial fracture repair: a novel method of surgical skills training using three-dimensional biomodels | Plastic Surgery |
| Davis, D | [23] | 2011 | The use of standardized patients in the plastic surgery residency curriculum: teaching core competencies with objective structured clinical examinations | Plastic and Reconstructive Surgery |
| Demirseren, ME | [24] | 2012 | Excised abdominoplasty material as a systematic plastic surgical training model | Plastic Surgery International |
| Ederer, IA | [61] | 2021 | A training model for local flaps using fresh human skin excised during body contouring procedures | Journal of Surgical Research |
| Farrell, DA | [36] | 2020 | Three-dimensionally-printed hand surgical simulator for resident training | Plastic and Reconstructive Surgery |
| Giurin, I | [37] | 2018 | A simulation model of nail bed suture and nail fixation: description and preliminary evaluation | Journal of Surgical Research |
| Gupta, S | [38] | 2018 | Innovative use of abdominoplasty specimen | Journal of Cutaneous and Aesthetic Surgery |
| Ibrahim, N | [39] | 2018 | A novel method for practising local skin flaps | Annals of the Royal College of Surgeons Edinburgh |
| Ji, C | [40] | 2016 | Plasticine model: a useful surgical training in plastic surgery | Aesthetic Plastic Surgery |
| Jovic, TH | [41] | 2020 | Using 3D printing technology to teach cartilage framework carving for ear reconstruction | Frontiers In Surgery |
| Kania, K | [42] | 2020 | Microsurgery training in plastic surgery | Plastic and Reconstructive Surgery – Global Open |
| Kantar, RS | [43] | 2020 | Knowledge and skills acquisition by plastic surgery residents through digital simulation training: a prospective, randomized, blinded trial | Plastic and Reconstructive Surgery |
| Kazan, R | [6] | 2017 | The evolution of surgical simulation: the current state and future avenues for plastic surgery education | Plastic and Reconstructive Surgery |
| Kazan, R | [44] | 2018 | The Montreal Augmentation Mammaplasty Operation (MAMO) simulator: an alternative method to train and assess competence in breast augmentation procedures | Aesthetic Surgery Journal |
| Kite, AC | [45] | 2018 | The use of a novel local flap trainer in plastic surgery education | Plastic and Reconstructive Surgery – Global Open |
| Lim, GH | [46] | 2020 | Evaluating the feasibility of a novel Marking Breast Oncoplastic Surgery Simulator (MBOSS) as a training tool for marking: a randomised trial | Gland Surgery |
| Loh, CYY | [47] | 2018 | Animal models in plastic and reconstructive surgery simulation - a review | Journal of Surgical Research |
| Mason, KA | [14] | 2016 | Twelve tips for postgraduate or undergraduate medics building a basic microsurgery simulation training course | Medical Teacher |
| Masud, D | [48] | 2017 | Microsurgery simulation training system and set up: an essential system to complement every training programme | Journal of Plastic, Reconstructive and Aesthetic Surgery |
| Nykiel, M | [25] | 2014 | An economical training model to teach and practice deep inferior epigastric artery perforator dissection | Annals of Plastic Surgery |
| Oezdogan, Y | [49] | 2020 | Perforator dissection simulation: a high-fidelity five-flap porcine training model | Journal of Maxillofacial and Oral Surgery |
| Pafitanis, G | [50] | 2017 | The chicken thigh adductor profundus-free muscle flap: a novel validated non-living microsurgery simulation training model | Archives of Plastic Surgery |
| Papavasiliou, T | [62] | 2021 | A standardized hand fracture fixation training framework using novel 3D printed ex vivo hand models: our experience as a unit | Plastic and Reconstructive Surgery – Global Open |
| Pfaff, MJ | [51] | 2016 | Plastic surgery resident understanding and education using virtual surgical planning | Plastic and Reconstructive Surgery |
| Podolsky, DJ | [52] | 2017 | Evaluation and implementation of a high-fidelity cleft palate simulator | Plastic and Reconstructive Surgery |
| Prsic, A | [53] | 2020 | A 3-dimensional-printed hand model for home-based acquisition of fracture fixation skills without fluoroscopy | Journal of Surgical Education |
| Riedle, H | [54] | 2019 | Design and fabrication of a generic 3D-printed silicone unilateral cleft lip and palate model | Journal of Plastic, Reconstructive and Aesthetic Surgery |
| Rinker, B | [19] | 2008 | Teaching patient selection in aesthetic surgery: use of the standardized patient | Annals of Plastic Surgery |
| Schendel, S | [17] | 2005 | A surgical simulator for planning and performing repair of cleft lips | Journal of Cranio- Maxillofacial Surgery |
| Soto-Miranda, MA | [26] | 2014 | Description and implementation of an ex vivo simulator kit for developing microsurgery skills | Annals of Plastic Surgery |
| Sullivan, SA | [27] | 2015 | Development of technical skills: education, simulation, and maintenance of certification | Journal of Craniofacial Surgery |
| Tejos, R | [8] | 2021 | Mind the gap: a competency-based scoping review of aesthetic and reconstructive reported simulation training models | Aesthetic Plastic Surgery |
| Thomson, JE | [55] | 2018 | Current status of simulation training in plastic surgery residency programs: a review | Archives of Plastic Surgery |
| Ur, R | [56] | 2016 | Development of a burn escharotomy assessment tool: a pilot study | Journal of Burn Care and Research |
| Wang, C | [57] | 2017 | A low-cost simulator for training in endoscopic-assisted transaxillary dual-plane breast augmentation | Annals of Plastic Surgery |
| Wang, X | [28] | 2015 | Skin simulators for dermatologic procedures | Dermatology Online Journal |
| Watt, DAL | [16] | 1999 | Simulating split-skin graft harvest | British Journal of Plastic Surgery |
| Weber, EL | [58] | 2017 | Preoperative surgical rehearsal using cadaveric fresh tissue surgical simulation increases resident operative confidence | Annals of Translational Medicine |
| Wilson, PA | [18] | 2001 | Surgical simulation in plastic surgery | British Journal of Plastic Surgery |
| Wu, SS | [63] | 2021 | Surgical simulation course for facial fracture education | Plastic and Reconstructive Surgery – Global Open |
| Zucca-Matthes, G | [59] | 2017 | Mastotrainer new version: a realistic simulator for training in breast surgery | The Breast |