
Effective teamwork remains a crucial component in providing high-quality care to patients in today’s complex healthcare environment. A prevalent ‘us’ versus ‘them’ mentality among professions, however, impedes reliable team function in the clinical setting. More importantly, its corrosive influence extends to health professional students who model the ineffective behaviour as they learn from practicing clinicians. Simulation-based training (SBT) of health professional students in team-based competencies recognized to improve performance could potentially mitigate such negative influences. This quasi-experimental prospective study will evaluate the effectiveness and impact of incorporating a multi-year, health science centre-wide SBT curriculum for interprofessional student teams. It targets health professional students from the Schools of Medicine, Nursing and Allied Health at Louisiana State University (LSU) Health New Orleans.
The intervention will teach interprofessional student teams key team-based competencies for highly reliable team behaviour using SBT. The study will use the Kirkpatrick framework to evaluate training effectiveness. Primary outcomes will focus on the impact of the training on immediate improvements in team-based skills and attitudes (Level 2). Secondary outcomes include students’ perception of the SBT (Level 1), its immediate impact on attitudes towards interprofessional education (Level 2) and its impact on team-based attitudes over time (Level 3).
The Institutional Review Board at LSU Health New Orleans approved this research as part of an exempt protocol with a waiver of documentation of informed consent due to its educational nature. The research description for participants provides information on the nature of the project, privacy, dissemination of results and opting out of the research.
Effective teamwork is a critical component of providing quality patient care. In a recent meta-analysis involving almost 1400 acute care teams, Schmutz et al.[1] found that high team performance was 2.8 times more likely in teams using team processes. This finding represented a positive, medium-sized effect between teamwork and clinical performance. In fact, improving team processes and behaviours with team training often results in improved care processes and patient outcomes [2].
Team performance, however, is far from ideal in healthcare today. An ‘us’ versus ‘them’ mentality permeates the clinical environment between professions and disciplines[3,4]. This tribalism leads to tensions due to conflicting expectations and the tendency for each profession to attribute ‘good’ traits to itself and ‘bad’ traits to other professions[5]. Furthermore, the silo-like nature of the episodic, speciality-based care structure [6] and each profession’s educational curricula [5] exacerbates these differences.
Such an environment inhibits effective communication within teams [7–9]. In addition, it harms safety climates in dynamic settings like the operating theatre (OR) [10,11]. It also produces differing views of effective collaboration between professions [12]. Thus, disruptions in care processes can occur due to incivility and bullying [13], or clinical inefficiencies develop due to over-controlling leadership practices [12].
An additional drawback to the ineffective teamwork arising in healthcare today is the negative influence it has on health professional students rotating in this environment. The seeming disrespect among professions, the hierarchical structure within the work environment and perceptions of superiority within some specialities can lead to negative role modelling that students mimic [14]. These cultural aspects of team interaction form a hidden curriculum that results in the adoption of values without much reflection or critique through ritualistic behaviours and symbolic stories [15].
Team training is an excellent means of inculcating students in the benefits of team-based competencies [16]. Its use with pre-licensure health professional students is effective in improving their team knowledge, communication and skills [17]. Baker et al. [18] demonstrated improvements in team leadership, situation awareness and overall communication among interprofessional teams of undergraduate health professional students in trauma resuscitation after a 15-minute intervention focusing on key components of the Agency for Healthcare Research and Quality (AHRQ)-developed Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS™) [14] program. In particular, these interprofessional student teams were better able to prioritize tasks and to work together to complete tasks after such training.
An especially effective modality for team training in healthcare is simulation-based training (SBT). It provides an opportunity for teams to learn team-based competencies in a safe learning environment without risk of harm to patients [19]. In addition, SBT allows teams to practise responding to high-risk, low-frequency events that may occur in the clinical setting [20]. In the acute care setting, interprofessional SBT of teams improves team processes and clinical outcomes [21–24]. In fact, high-fidelity SBT is a particularly common modality for healthcare team training overall [25]. It is also a popular modality for training pre-licensure health professional student teams [18]. Health professional students participating in team-based SBT find such experiences give insight into their personal reactions, their own team performance and their lack of ability in team competencies [26]. Notably, it makes these students want to participate in more interprofessional team training [27]. Given these facts, SBT is an ideal modality for training interprofessional health professional teams in teamwork.
Previous works by the authors have demonstrated that using high-fidelity SBT to teach interprofessional student teams is feasible and effective for both junior and senior pre-licensure students as well as postgraduate learners in medicine, nursing and allied health [27–32]. Such endeavours, however, were either small in scale or limited in time. Thus, its impact was restricted to a minority of health professional students or within a year framework. To understand the dynamics of a larger implementation of such high-fidelity SBT, we will investigate the integration of such training at a health science centre-wide level over several years. We hypothesize that interprofessional student SBT of teams incorporating medicine, nursing and allied health will improve participants’ knowledge, skills and attitudes towards teams and teamwork.
The study is a prospective, quasi-experimental pre-/post-intervention comparison design in which participants act as their own controls by completing evaluations before and after the team training intervention. SBT sessions will take place over a 3-year period, initially focusing on students within the Schools of Medicine (SOM) and Nursing (SON). Over the SBT training period, participants will expand to include students from the School of Allied Health (SOAH). Table 1 provides a detailed listing of the key elements, components and descriptions of the SBT activity.

| Elements | Components | Descriptions |
|---|---|---|
| Participant orientation | ||
| To the simulator | Upon completion of initial surveys, participants come into the learning environment with computerized mannequin on gurney in central part of the room. The facilitator invites them to gather around the mannequin to start the approximately 5-minute orientation. After introductions of faculty, the facilitator reviews the goals of the simulation-based training (SBT) and ground rules for the session. During this time, the participants are asked whether they are familiar with the mannequin and how it functions. If they are not familiar with it, the facilitator will introduce the participants to the mannequin, describing how it responds to inputs in the same physiological manner as a human. The facilitator also emphasizes that the mannequin, although realistic in many ways, is still made out of plastic and may at times respond inappropriately, not be able to respond or malfunction during the session. The participants are encouraged to not let such events distract them but act, instead, as they would in real life to the situations they encounter. | |
| To the environment | During the orientation, the facilitator also points out the equipment available to the participants in the room. In addition, the facilitator explains that faculty may be in the room at the time of the session but that the participants should ignore their presence and not direct any inquiries to them. The participants are reminded that the faculty will not respond to questions, but faculty will give information to the students as required due to limitations or malfunctions of the mannequin. | |
| Simulator type | ||
| Make and model | For the SBT, a human patient simulator (HPS) computerized mannequin is the patient. We use multiple makes and models, from wireless to older cabled versions. | |
| Functionality | The HPS has the full array of physiologic responses to interventions and conditions encountered during the SBT. It has a software interface developed at our institution to allow for one-touch changes in multiple parameters, improving ease of use. For example, in one scenario, clicking on one such button will change blood pressure, heart rate and respiratory status to reflect stage 2 hypovolemic shock. The interface also has pre-set verbal responses that are activated according to questions to the mannequin by the participants and clinical scenario. Limitations to the simulator include the inability to perform certain procedures on it, such as central line placement or arterial line placement. Additionally, the clumsiness of scanning drugs makes it ineffective. Consequently, participants must announce the drugs that they give. | |
| Simulation environment | ||
| Location | SBT sessions take place at the LSU Health New Orleans School of Medicine in specialized simulation rooms housing the HPS. Based on the room used, simulator operators may conduct the scenarios from a control room with one-way glass or off to the side of the mannequin in the room itself. | |
| Equipment | For each scenario, available equipments for the participants include the following: an intravenous starter kit, intravenous fluid with tubing, an ambu bag with tubing, an oral airway, a nasopharyngeal airway, an endotracheal tube, an Eschmann stylet, a laryngoscope with Miller blade and Macintosh blade, syringes, face mask, oxygen nasal cannula, 15 blade scalpel, a spinal needle, a thoracostomy tube and a fully stocked code cart. The airway, intravenous and thoracostomy equipments are located on a side table near the head of the bed of the patient. The code cart is in the corner at the back of the simulation room. A ventilator is optional if available. | |
| External stimuli | No external stimuli are part of the scenario | |
| Simulation event/scenario | ||
| Event description | Over the course of the 3 years, the project will employ six scenarios that each focus on a particular behavioural health issue with a specific medical emergency situated in either an Emergency Department (ED) or Intensive Care Unit (ICU) setting (see Table 2 for descriptions of each). The project will develop two scenarios per year. Each scenario will catalyze the need for highly reliable teamwork through the development of an emergent medical problem requiring prompt intervention and treatment. For each scenario, the software interface will provide the opportunity for real-time HPS response to team treatment decisions through one-touch controls. For example, proper decompression of a tension pneumothorax (i.e., via needle or thoracostomy placement) will result in physiological improvement and resolution of the condition. Inadequate therapy will result in continued decomposition of physiological status and parameters. | |
| Learning objectives | On completion of the SBT session, students will be able to | |
| 1. Differentiate effective from ineffective teamwork behaviours and their relation to the following team-based competencies: shared mental model, situation awareness, cross monitoring, open communication, resource management, anticipatory response, flattened hierarchy, role clarity and mental rehearsal. | ||
| 2. Practise highly reliable teamwork during an SBT crisis scenario using one or more of the following team-based competencies: shared mental model, situation awareness, cross monitoring, open communication, resource management, anticipatory response, flattened hierarchy, role clarity and mental rehearsal. | ||
| 3. Identify behavioural health disorders such as post-traumatic stress disorder (PTSD), alcohol and drug abuse, depression and traumatic brain injury-associated disorders through the use of evidence-based screening modalities | ||
| 4. Recognize and initially treat potentially life-threatening conditions such as tension pneumothorax, cardiac arrhythmias, seizure, delirium tremens and PTSD-induced emergence agitation. | ||
| Participant composition | Each SBT session will involve interprofessional student teams consisting of a combination of nurse anaesthesia students, senior medical students, respiratory therapy students, occupational therapy students and physical therapy students. | |
| Adjuncts | Props for the SBT will include the equipment described as part of the simulation environment. | |
| Facilitator/operator characteristics | Clinical faculty from the Schools of Medicine, Nursing and Allied Health will serve as facilitators, simulation operators and assessors for the SBT. Operators will have familiarity with the software interface used to control the HPS. At least two facilitators will assist with the debriefing. If possible, each facilitator should be faculty from a different profession to model interprofessional collaboration. | |
| Pilot testing | After the development of each scenario, faculty will conduct at least one pilot session to identify and address glitches and impediments to its smooth running. If necessary, additional pilot sessions will occur to ensure seamless implementation of each scenario during SBT sessions. | |
| Embedded educators/simulated patients | No simulated patients or embedded educators are part of the scenarios | |
| Instructional design | ||
| Duration | Sessions will involve a two-scenario format lasting 2 hours in total time. | |
| Timing | Initial data collection involving surveys for the participants will occur at the beginning of the session. The participants will then undergo orientation and conduct the first scenario during which time assessors will observe and rate performance. After the initial debriefing, participants will perform self- and peer-assessment of performance. Participants then will perform the second scenario during which time assessors will again observe and rate performance. After the second debriefing, participants will conduct self- and peer-assessment of performance and then complete post-session surveys. | |
| Frequency/repetitions | Every participant will complete at least one SBT session in which teams will complete two separate scenarios for reinforcement of learning. | |
| Clinical variation | As described under the scenario event description, six separate scenarios involving a specific behavioural health disorder and a particular emergent medical problem will serve to provide clinical variation. | |
| Standards/assessment | Participants will be novices related to teamwork and the use of team-based competencies. Their experience with behavioural health disorders and the emergent medical conditions encountered will vary based on their profession and prior clinical experience. Assessments will include measures of attitudes towards interprofessional education and teamwork as well as evaluation of team performance (see text). | |
| Adaptability of intervention | During the second scenario, each participant will practise a specific team-based competency that he/she will choose to work on at the end of the first debriefing. In this manner, participants will individualize their learning to focus on those aspects of teamwork that they would like to practise. | |
| Range of difficulty | The SBT scenario design will involve behavioural health issues and emergent medical conditions chosen to be similar in difficulty and complexity. | |
| Non-simulation interventions and adjuncts | Participants will not receive any pre-session instruction or assignments. In this manner, their experience during the first scenario will help them identify gaps in their performance and instil the need to know how to improve them as well as the motivation to work on them critical in adult learning. | |
| Integration | SBT sessions will integrate into existing curricula of students from each of the participating schools to help with logistics, faculty participation and reach. | |
| Debriefing | ||
| Source | Debriefings will involve facilitators. | |
| Duration | Debriefings will last approximately twice as long as a scenario (30 minutes to 15 minutes). | |
| Facilitator presence | At least two facilitators, ideally from different professions, will lead the debriefing. | |
| Facilitator characteristics | Facilitators will include faculty from the Schools of Medicine, Nursing and Allied Health. Each facilitator will undergo faculty development by participating in an approximately 3-hour seminar. Novice facilitators will pair with more experienced facilitators during their initial sessions to observe and receive feedback. | |
| Content | The content of the debriefing reflects the learning objectives. It will include discussion and review of team-based competencies and how they relate to effective and ineffective team performance, behavioural health disorders and how to screen for them and the initial treatment of emergent medical conditions. | |
| Structure/method | The orientation to the SBT session will serve as a pre-brief. Debriefings themselves will follow reaction, analysis and application phases. The facilitators will use various techniques to enhance learning during the debriefings including Thiagi’s six phases [33], Pearson and Smith’s three questions [34] and plus/delta [35]. | |
| Timing | Debriefings will occur immediately following the completion of a scenario and will take place within the simulation environment to assist participants with recall and allow for demonstration of competencies. | |
| Video | Each SBT scenario will undergo video recording, but debriefing will only refer to it to resolve disputed actions/events between participants that disrupt smooth flow of the debriefing | |
| Scripting | Although facilitators will not use a formal script during debriefing, each debriefing will begin with the question ‘How did that feel’? and facilitators will address the nine key team-based competencies as well as elicit from participants a commitment to work on at least one of them in clinical practice. |
The aim of the project is to teach interprofessional student teams key team-based competencies recognized to enhance team performance through an SBT format. Primary research objectives include the following: (1) to determine the extent to which SBT of interprofessional student teams immediately impact participants’ team-based behaviours in a simulated environment and (2) to determine the extent to which SBT of interprofessional student teams immediately impact participants’ team-based attitudes in a simulated environment. Secondary research objectives include the following: (1) to determine the extent to which student teams react to SBT sessions, (2) to determine the extent to which SBT of interprofessional student teams influences participants’ attitudes to interprofessional education and (3) to determine the extent to which SBT of interprofessional student teams impacts participants’ team-based attitudes over time.
The SOM, SON and SOAH are all co-located on the LSU Health New Orleans main campus situated near its central business district. Training sessions will take place at the LSU Health New Orleans School of Medicine Learning Center, a 30,000 square foot, two-floor simulation centre located on this main campus. Sessions will occur in rooms dedicated to high-fidelity SBT. Each room has a full-scale, computer-operated human patient simulator (HPS) mannequin (CAE, Inc., Montreal, Canada) to serve as the scenario’s ‘patient’. Each room will serve as a patient room in either the emergency department or intensive care unit, depending upon the SBT scenario. Teams will have equipment available typically used by rapid response or cardiac arrest teams to resuscitate deteriorating patients, such as airway resuscitation equipment, code cart, cardiac defibrillator, intravenous catheters and fluids and thoracostomy tubes.
Figure 1 outlines the format followed for each SBT session. Each session will begin with an orientation to the session in which the facilitators will show the participants the simulator and training setting, review the objectives of the session, provide ground rules and introduce participants to the scenario background. Following this pre-brief, participants will then undergo a first scenario in which the simulated patient will suddenly deteriorate, prompting the need for team resuscitation of the patient. Immediately following this first scenario, facilitators will guide an after-action structured debriefing focusing primarily on nine team-based competencies: shared mental model, situation awareness, cross monitoring, open communication, resource management, anticipatory response, flattened hierarchy, role clarity and mental rehearsal. It will also include a review of key aspects of clinical care and a discussion related to military veteran behavioural health issues commonly encountered by providers. The debriefing will follow established techniques to enhance learning, including Thiagi’s six phases of debriefing, Pearson and Smith’s three questions [33] and the plus/delta technique [34]. Participants will then do a second scenario involving a different patient crisis to practise lessons learned. A second debriefing will immediately follow the completion of the second scenario, expanding on themes related to teamwork and applications to the clinical setting. The second debriefing and the session will conclude with a summary and an elicitation of a commitment from each participant to employ one of the team-based competencies in clinical practice.

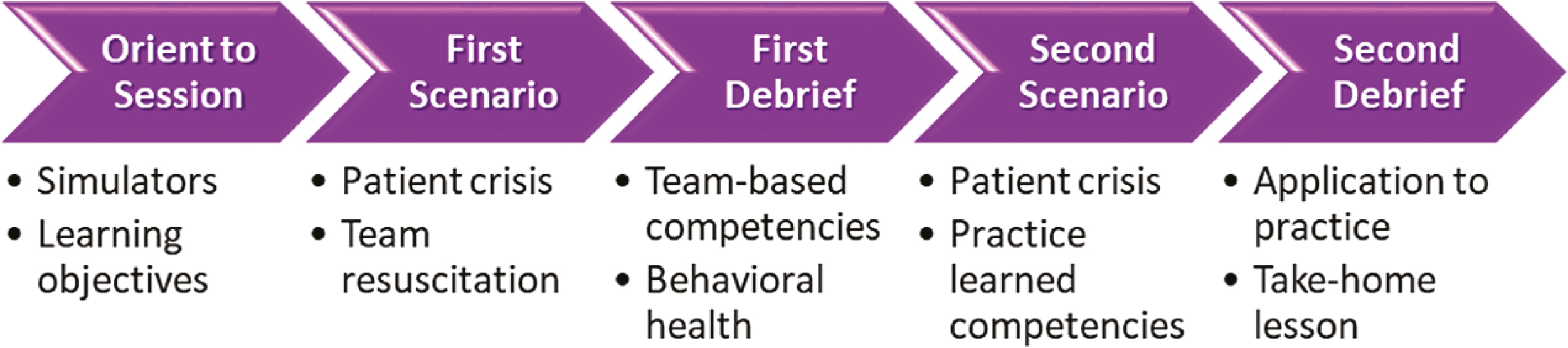
Simulation-based training session dual scenario format.
Participants for the SBT sessions will consist of interprofessional teams of senior medical students, second- and third-year nurse anaesthesia students, physical therapy students, occupational therapy students and respiratory therapy students. Team composition will evolve over the course of implementation. In the first year, they will consist of senior medical students and nurse anaesthesia students. For the following academic year, teams will transition to senior medical students, nurse anaesthesia students and occupational therapy students. In the final academic year of implementation, physical therapy students and respiratory therapy students will begin to participate in teams with senior medical students and nurse anaesthesia students.
Interprofessional student teams will consist of six members, two members from each of the professions participating in the SBT session. Within each profession, one member will assume a senior role with the other playing a junior role for the first scenario; they will then switch the roles for the second scenario. In situations where fewer or more team members participate in an SBT session, removal of the junior role or addition of other mid-level roles will occur, respectively.
Training scenarios will focus on a patient with a behavioural health disorder who undergoes rapid clinical deterioration due to an underlying illness, such as pneumothorax or unstable atrial fibrillation (Table 2). Scenarios will, therefore, create a clinical situation leading to the need for a rapid response or code resuscitation of the patient. This design serves to catalyse team interaction among the participants to care for the patient. In this way, participants will have to function effectively as a team to resuscitate the patient, producing rich content for discussion during the after-action, facilitator-guided structured debriefing that will introduce to participants the team-based competencies characteristic of highly reliable team performance. The scenarios will employ a user-friendly, easy-to-use, interactive software developed in-house [28,31].

| Scenario Patient name, age, gender and background | Medical condition leading to resuscitation | Behavioural health disorder | Background setting to start scenario | Medical treatment required to resuscitate patient | Behavioural health screening reviewed | Projected starting year |
|---|---|---|---|---|---|---|
| Ben Cooper 75-year-old male Vietnam veteran who has just undergone coronary artery bypass grafting for coronary artery disease |
Emergence delirium | Post-traumatic stress disorder (PTSD) | Post-operative setting awaiting extubation after transfer from operating room (OR) to intensive care unit (ICU) | Re-orient patient, call additional staff, perform neurologic exam, administer dexmetomidine hydrochloride or ketamine for PTSD_induced delirium | PTSD screening | Year 1 |
| Pre-operative treatment (Rx) – assessment & plan | ||||||
| Intra-operative Rx – anaesthesia selection | ||||||
| Post-op Rx – low stimulation, pain control, avoid touch, document | ||||||
| Michael Blackwood 39-year-old male smoker who became short of breath while working out at the gym |
Spontaneous Pneumothorax | PTSD | Emergency Department (ED) | Needle decompression, chest tube insertion | PTSD screening | Year 1 |
| Clara Cetkin 36-year-old homeless female found down with blood alcohol (EtOH) level of 0.2 mg/dL and + cocaine screen |
Disorientation | PTSD, Substance Abuse | ICU | Delirium tremens (DT) Rx, Ventricular dysrhythmia Rx | PTSD screening | Year 2 |
| EtOH/drug abuse screening with CAGE Questionnaire, Alcohol Use Disorders Identification Test (AUDIT-C) | ||||||
| Captain Marquis Blade 28-year-old schizophrenic, homeless male Afghanistan War veteran who presents with chest pain |
Unstable atrial fibrillation (AF) | PTSD | ED | Unstable AF Rx, PTSD Rx | PTSD screening | Year 2 |
| Private John Lee 24-year-old male Afghanistan War veteran with history of traumatic brain injury (TBI) who collapsed on street & was unresponsive |
TBI and seizure | Multiple co-occurring conditions | ED; wife arrives later and provides history | Control seizure, stabilize patient, neurologic exam, order diagnostic tests | Differences between mild, moderate & severe TBI, complications & Rx | Year 3 |
| Bob Ryan 28-year-old male who jumped from a bridge & is in ICU recovering from an open reduction, internal fixation of his femur |
Pneumothorax, Ventricular tachycardia (V-tach) | Depression, PTSD | ICU | Insert chest-tube, Rx V-tach | Generalized Anxiety Disorder-7 GAD-7); Patient Health Questionnaire-2 (PHQ-2, PHQ-9); PTSD screening | Year 3 |
An enhancement of the scenario design will include starting the scenarios with only part of the interprofessional team in the patient room. Two members of the same profession will serve as the initial caregivers who will start the scenario at the patient’s bedside. These team members will receive the background information regarding the scenario. The other caregivers will remain outside of the patient room out of sight and sound of any interactions between the initial caregivers and the patient. Thus, the initial caregivers will evaluate the patient condition, perform any necessary screening evaluations, recognize any deterioration and call in the rest of the team members at the appropriate time. In addition, these initial caregivers will need to update the other team members on the patient background and events leading up to the call in. This design will enhance the need for effective team interaction and function in order for the team to resuscitate the patient.
Outcome measures will follow the Kirkpatrick framework for the assessment of training effectiveness [35]. Table 3 summarizes the evaluation techniques and instruments proposed for each level of training effectiveness and the timing of their use. Collection of Level 1 data will occur at the end of each session through verbal enquiries.

| Kirkpatrick level | Type of method | Description of evaluation | Rating scale | Time obtained |
|---|---|---|---|---|
| Level 1 Reaction (secondary outcome) | Qualitative – verbal questions asked to all participants of a session | Questions asked: | Interpretation of verbal responses replying to questions | Asked at the session end after debrief |
| Was this worthwhile? | ||||
| Why or why not? | ||||
| How can we improve the scenarios/session? | ||||
| Level 2 Learning (primary outcome) | Quantitative – observer- and participant-based assessment instruments | Teamwork Assessment Scales (TAS) – 11 item tool with three subscales: 1) team-based behaviours (TBB) – a 5-item multisource evaluation (MSE) of individual performance; 2) shared mental model (SMM) – a 3-item evaluation of aspects of overall team performance; and 3) Adaptive communication and response (ACR) – a 3-item evaluation of aspects of overall team performance | 6-point Likert type scale – 1 = definitely No to 6 = definitely Yes | Completed by at least two observers and each participant after each scenario and debriefing cycle |
| (secondary outcome) | Readiness for Interprofessional Learning Scale (RIPLS) questionnaire – 19-item instrument measuring participant student attitudes to interprofessional learning | 5-point Likert scale – 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree | Completed by each participant right before beginning of training session and right after completion of training session | |
| Some reverse rating items | ||||
| (primary outcome) | Interprofessional Teamwork (IPT) questionnaire – 15-item instrument measuring participants’ interprofessional teamwork self-efficacy | 6-point Likert type scale – 1 = Definitely No to 6 = Definitely Yes | Completed by each participant right before beginning of training session and right after completion of training session | |
| Level 3 Behaviour Change (secondary outcome) | Quantitative – participant self-report instrument | TeamSTEPPSTM Teamwork Attitude Questionnaire (T-TAQ) – 30-item instrument divided into five subscales of six questions each – 1) Team structure, 2) Leadership, 3) Situation monitoring, 4) Mutual support, 5) Communication | 5-point Likert scale – 1 = Strongly disagree, 2 = Disagree, 3 = Neutral, 4 = Agree, 5 = Strongly Agree | Given to the senior medical school class at the beginning of their final academic year in June and right before graduation from medical school in April of that academic year |
| Level 4 Outcomes | Not measured |
The Teamwork Assessment Scales (TAS) is an 11-item, 3 subscale, Likert-type instrument that participants and observers will complete after each scenario. This tool has evidence of both convergent validity [29] and generalizability [28]. It will assess performance improvement over the course of the SBT session. The Readiness for Interprofessional Learning Scale (RIPLS) questionnaire is a 19-item, Likert scale instrument [36], widely used in the literature [37], that has undergone subscale modification [38]. Participants will complete it at the beginning and end of each session to evaluate the change in attitudes towards interprofessional education that occur as a result of the SBT intervention. The Interprofessional Teamwork (IPT) questionnaire [28,31] is a 15-item, Likert-type scale that participants will complete at the beginning and end of each session. It will evaluate the change in attitudes towards team-based competencies that occur during the SBT.
The TeamSTEPPS™ Teamwork Attitudes Questionnaire (T-TAQ) is a 30-item, 5 subscale, Likert scale instrument that has undergone scale reliability and correlation testing [39,40]. Students will complete this survey at the beginning and the end of the academic year in which they will participate in the SBT sessions. The T-TAQ will measure the change in attitudes towards teamwork over the course of the year, serving as a surrogate for behaviour change.
For each survey, students will use a personal identification number (PIN) that they self-generate to match pre-/post-intervention evaluations as well as to compare with other evaluations that the students complete. The TAS, RIPLS and IPT questionnaires will be completed using a tablet-based method that will allow direct input of data into the database, bypassing potential errors in transcription of data.
As an educational endeavour, all senior medical students and junior and senior nurse anaesthesia students will participate in the SBT sessions. They will have this opportunity because the team training will be incorporated into the curricula of both learner groups. Students participating from the School of Allied Health will participate as available based on their class schedules. The data, therefore, will constitute the equivalent of a convenience sample.
Analysis of Level 1 data will involve having at least two investigators evaluate themes related to responses given by participants independently. They will then reach an agreement together for verification. The resultant themes will serve as reaction data from the participants.
Analysis of Level 2 data will involve a comparison of mean item scores from pre-/post-intervention periods. For the TAS, mean subscale scores for observer and participant ratings will be determined for all first-time participants with one-way analyis of variance (ANOVA) evaluating the difference between the mean calculated observer- and participant-rated performances after each scenario for each year of the programme. For the RIPLS, the mean item scores will be determined, and paired samples t-test with Bonferroni correction will be calculated for each matched pre-/post-session item score for each year of the programme. Finally, for the IPT questionnaire, mean scores for each item will be determined and paired samples t-test with Bonferroni correction will be calculated for each matched pre-/post-session item score.
Analysis of Level 3 data will involve a comparison of T-TAQ scores from the beginning of the academic year of the SBT to the end of that same academic year. The mean T-TAQ subscale scores will be determined for each year of the programme, and one-way ANOVA will be calculated to evaluate the difference between mean calculated student scores. Finally, trends in subscale scores from year to year of each class of students will be analysed using linear regression.
For each statistical analysis, any incomplete paired data set will be discarded prior to comparison using an ad hoc method.
This project is a 3-year intervention funded by the United States Health Resources and Services Administration (HRSA). It was part of an HRSA 14-066 Advanced Nursing Education (ANE) Program Grant Award (No. D09HP26947).
The Institutional Review Board at LSU Health New Orleans approved this research as part of an exempt protocol with a waiver of documentation of informed consent due to its educational nature. The research description for participants provides information on the nature of the project, privacy, dissemination of results and opting out of the research. Participants’ completion of the surveys and questionnaires implied informed consent. Participants could have their data removed from research analysis, and they could opt-out at any time during the intervention.
All data will be protected in secure locations. Participants will create their own unique PIN using a set formula that they will use throughout the intervention period. This PIN will protect their identities while allowing matching of TAS, RIPLS, IPT questionnaires and T-TAQ data to allow for analysis of individual changes across all measurements.
Dissemination of results will focus on presenting research findings at medical education and simulation-based healthcare conferences through oral and poster formats. In addition, faculty development workshops will serve to prepare other instructors. Finally, publication of findings will occur in targeted peer-reviewed journals.
This project has several potential benefits for the research community. First, it will provide a template for incorporating interprofessional student team SBT into existing curricula at a large health sciences centre. The lessons learned in addressing the logistical and implementation challenges of such a large project will serve as invaluable pearls for other institutions attempting similar endeavours. Second, this project will involve a large number of student learners over the 3 years. As such, it will provide valuable information into the effectiveness of mass implementation of SBT in teamwork given over an academic year. Third, a secondary outcome will attempt to gain insight into long-term changes in attitudes/behaviours by looking at changes in teamwork attitudes over the course of the academic year. This information will shed light on the lasting impact of team-based SBT.
Challenges to implementation of this project include coordination of schedules between the various professional schools involved. Technical issues related to the tablet-based questionnaire system could also present problems will data collection. Given the number of participants who will undergo SBT, accommodations may be needed to have everyone trained. Finally, the curriculum and scenarios will need continuous evaluation and revision to address any issues encountered during the programme’s implementation.
In conclusion, this project provides an opportunity to evaluate the effectiveness of an SBT intervention to teach interprofessional students in team-based competencies. It will shed light on participant reactions to the training, learning related to team-based performance and attitudes, attitudinal change related to interprofessional education and long-term changes in teamwork attitudes. As such, it will help advance the field of team science in healthcare education.
The authors would like to thank all the health professional students who participated in the simulation-based training sessions over the three-year period of this project.
Drs. Bonanno, Paige, Garbee, and Yu participated in the study conception and design. All authors except for Dr. Yu will serve as faculty for sessions and collect data. Drs. Yu, Bonanno, Paige, and Garbee will participate in data analysis. Dr. Paige composed the draft manuscript, and all authors contributed to its critical revision.
A Health Resources and Services Administration (HRSA) – 14-066 Advanced Nursing Education (ANE) Program Grant Award (No. D09HP26947) provided support for the work described in this manuscript.
Data and materials are available upon reasonable request to Dr. Laura Bonanno, principal investigator.
Ethical approval for this project was obtained from the LSU Health New Orleans Health Sciences Center Institutional Review Board as an amendment to an exempt status project, No. 7101, looking at the impact of simulation-based team training which began in 2008. The research description for participants provides information on the nature of the project, privacy, dissemination of results and opting out of the research.
Dr. Paige receives royalties from Oxford University Press and Springer Nature for three books relating to simulation or surgical education. He also is a consultant to Boston Scientific as a faculty instructor. Finally, he receives grant support from the Southern Group on Educational Affairs (SGEA) and the International Association of Medical Science Educators (IAMSE) as PI for teamwork research as well as from Avita Medical as a co-investigator for hernia research. Drs. Bonanno, Garbee, and Yu are co-investigators on the SGEA and IAMSE grants. Drs. Bonanno and Garbee also receive royalties from Springer Nature for a book related to simulation. The remaining authors do not have any disclosures.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.